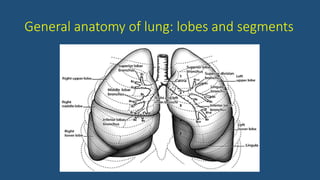
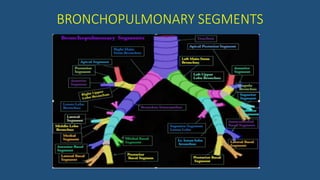
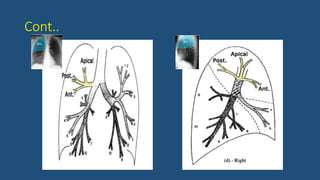
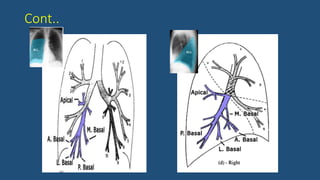
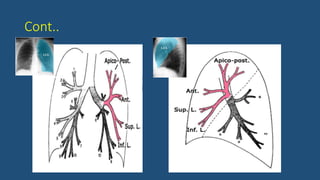
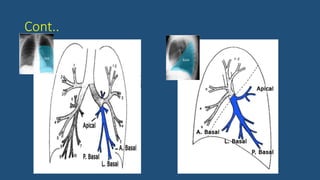
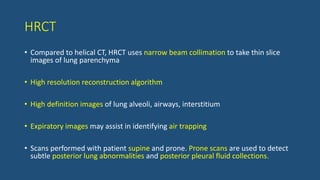
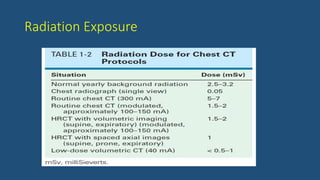
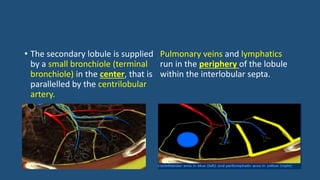
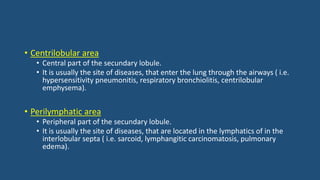
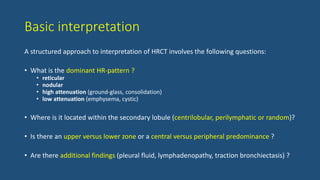
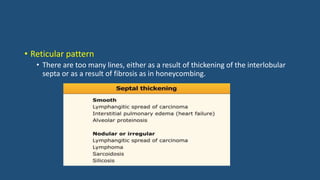
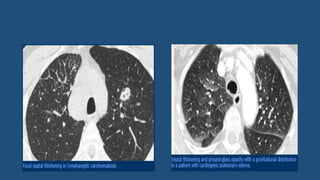
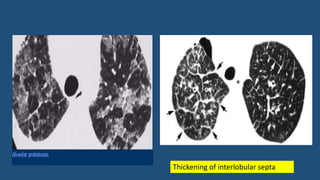
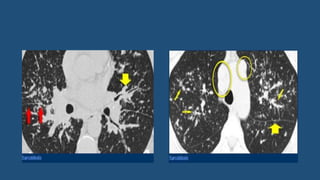
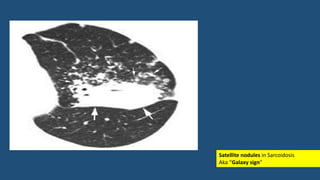
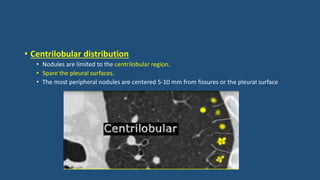
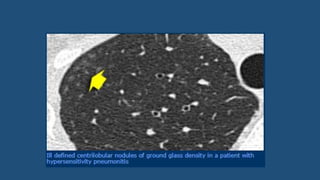
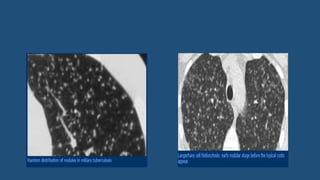
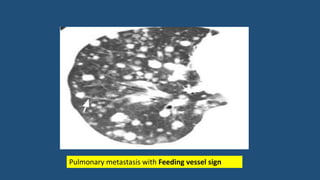
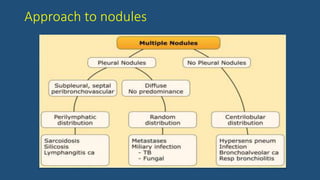
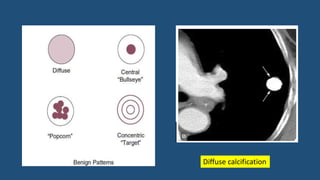
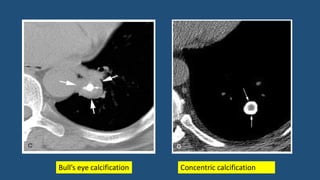
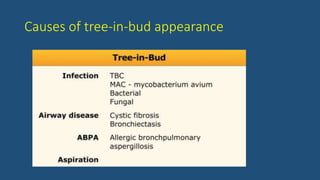
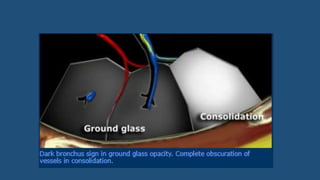
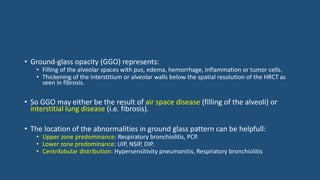
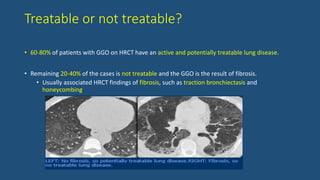
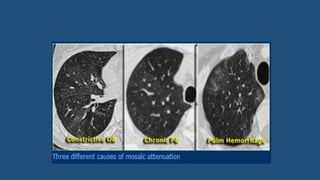
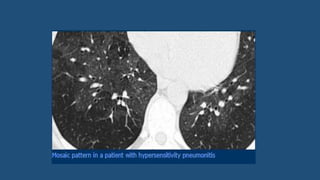
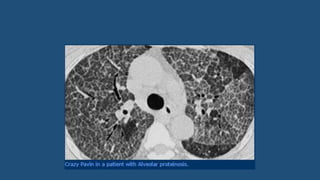
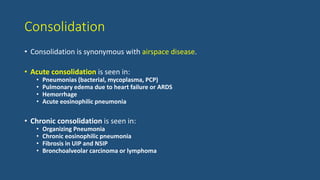
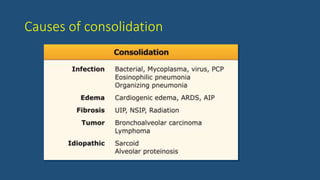
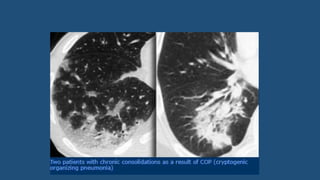
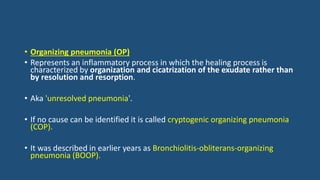
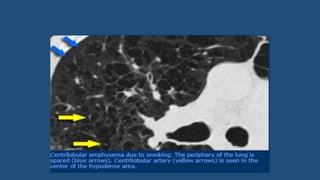
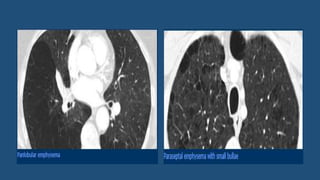
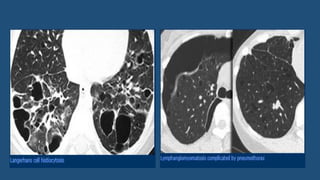
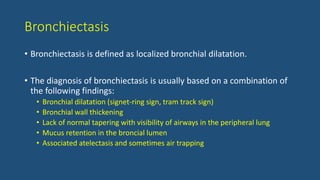
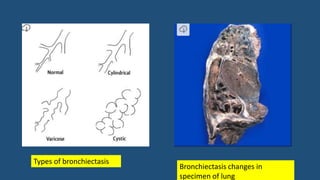
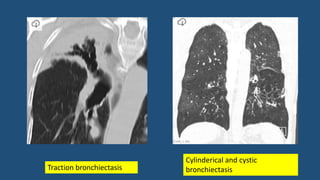
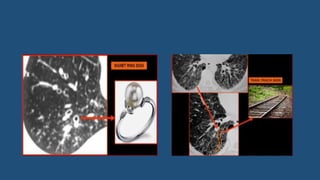
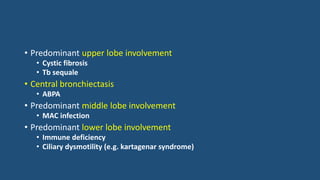
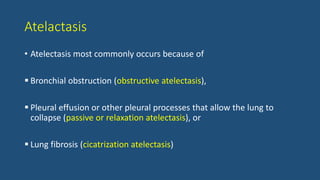
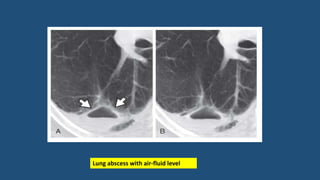
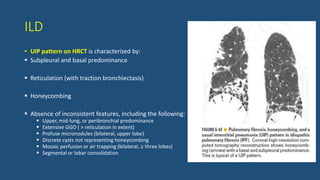
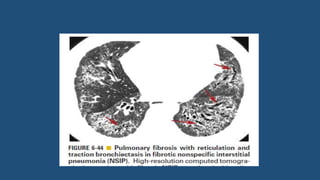
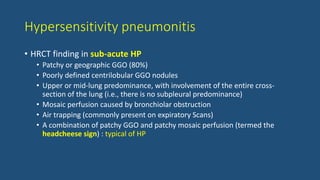
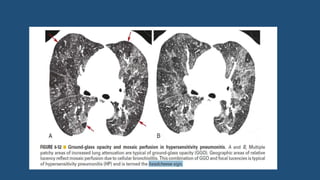
This document provides an overview of CT imaging of the chest and interpretation of lung pathology. It discusses lung anatomy, bronchopulmonary segments, and the mediastinum. It then covers the utility of CT chest for evaluating lung diseases, different CT protocols, and interpretation of common lung patterns including reticular, nodular, ground glass, consolidation, emphysema, cysts and bronchiectasis. Key aspects of the secondary lobule and structured approach to HRCT interpretation are also summarized.