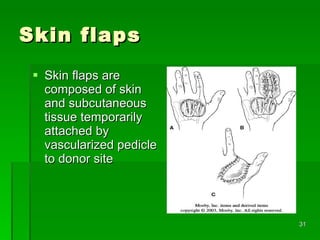
The document discusses various types of skin grafts and flaps used in orthopedics. It describes split thickness skin grafts which contain part of the epidermis and dermis and are useful for covering defects when the area is too wide for a full thickness graft. It also discusses axial pattern flaps which contain a direct cutaneous artery and allow coverage of the hand while preserving movement. Local flaps are preferred over distant flaps when possible due to better color and texture matching and reduced risk of complications.