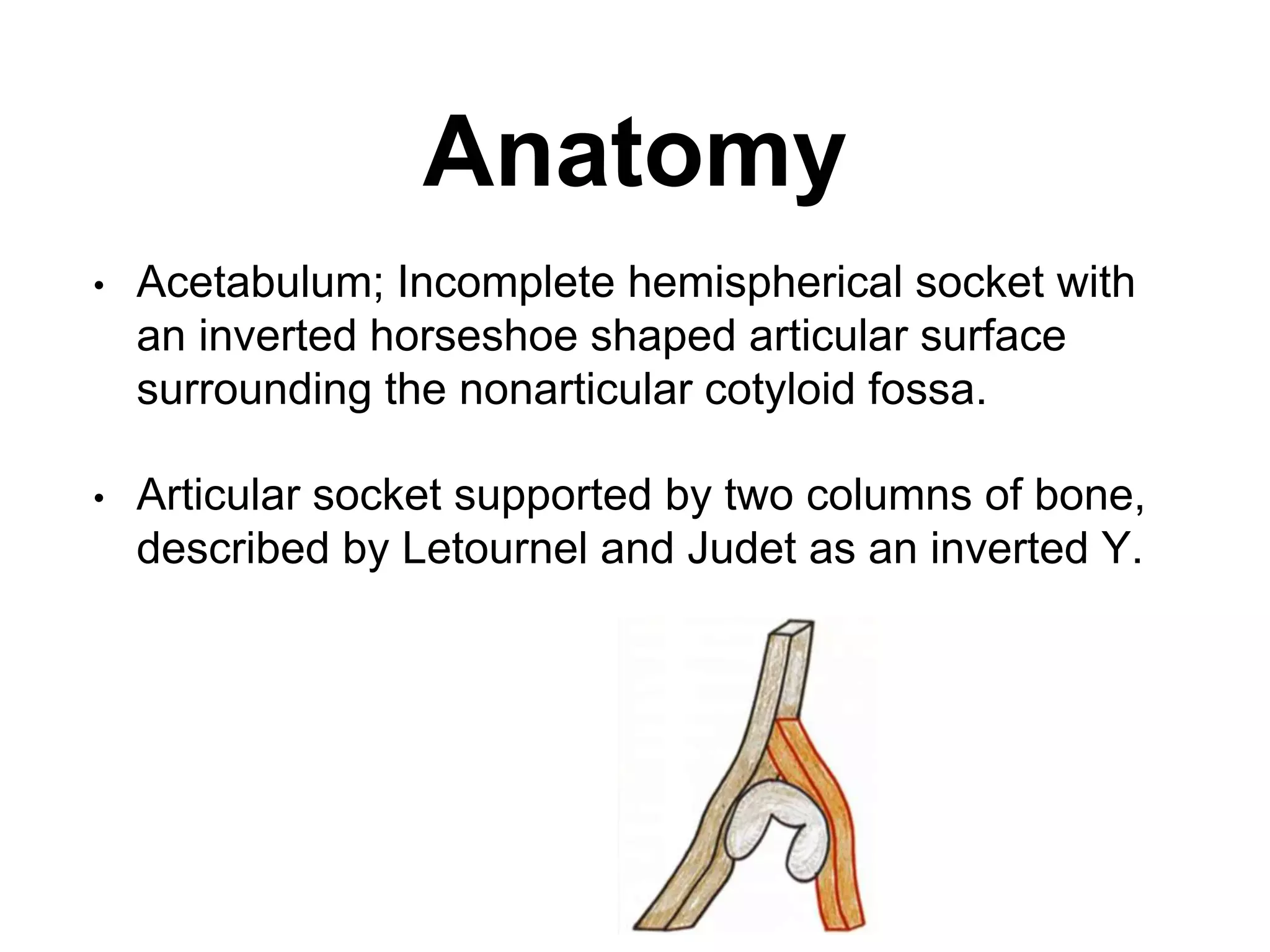
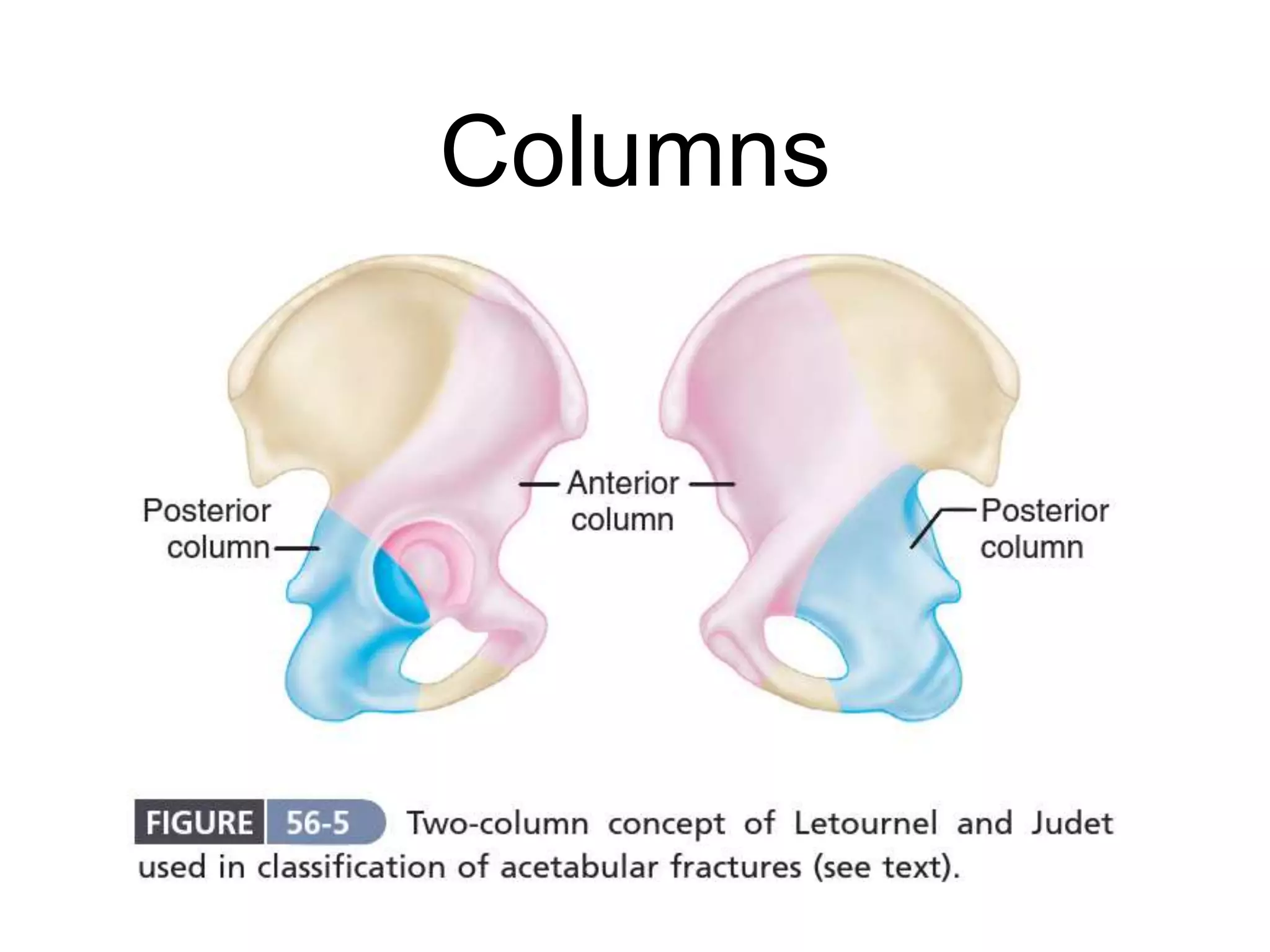
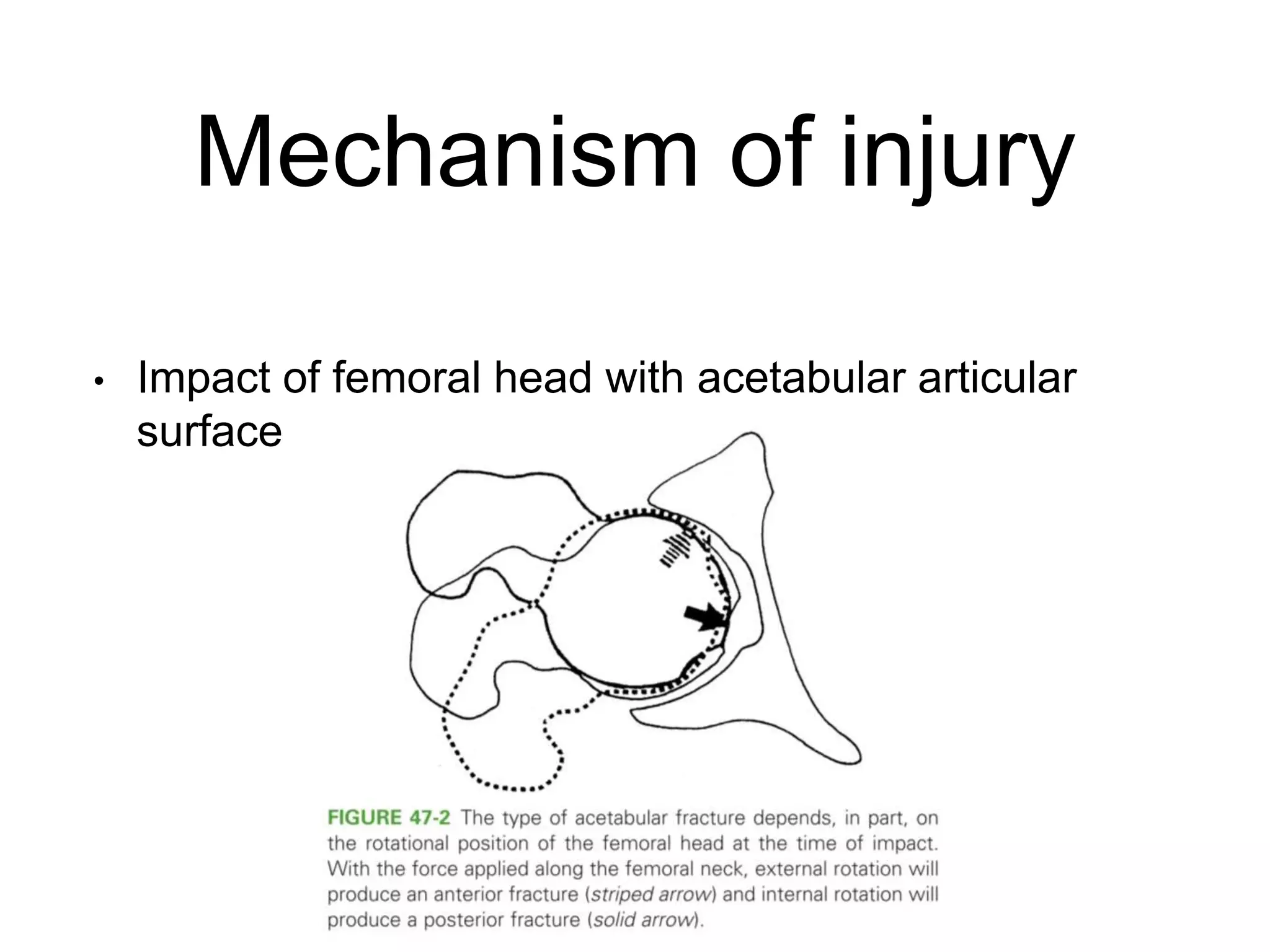
1) Acetabular fractures are caused by high-energy trauma and require complex treatment due to the anatomy of the acetabulum and risk of joint instability.
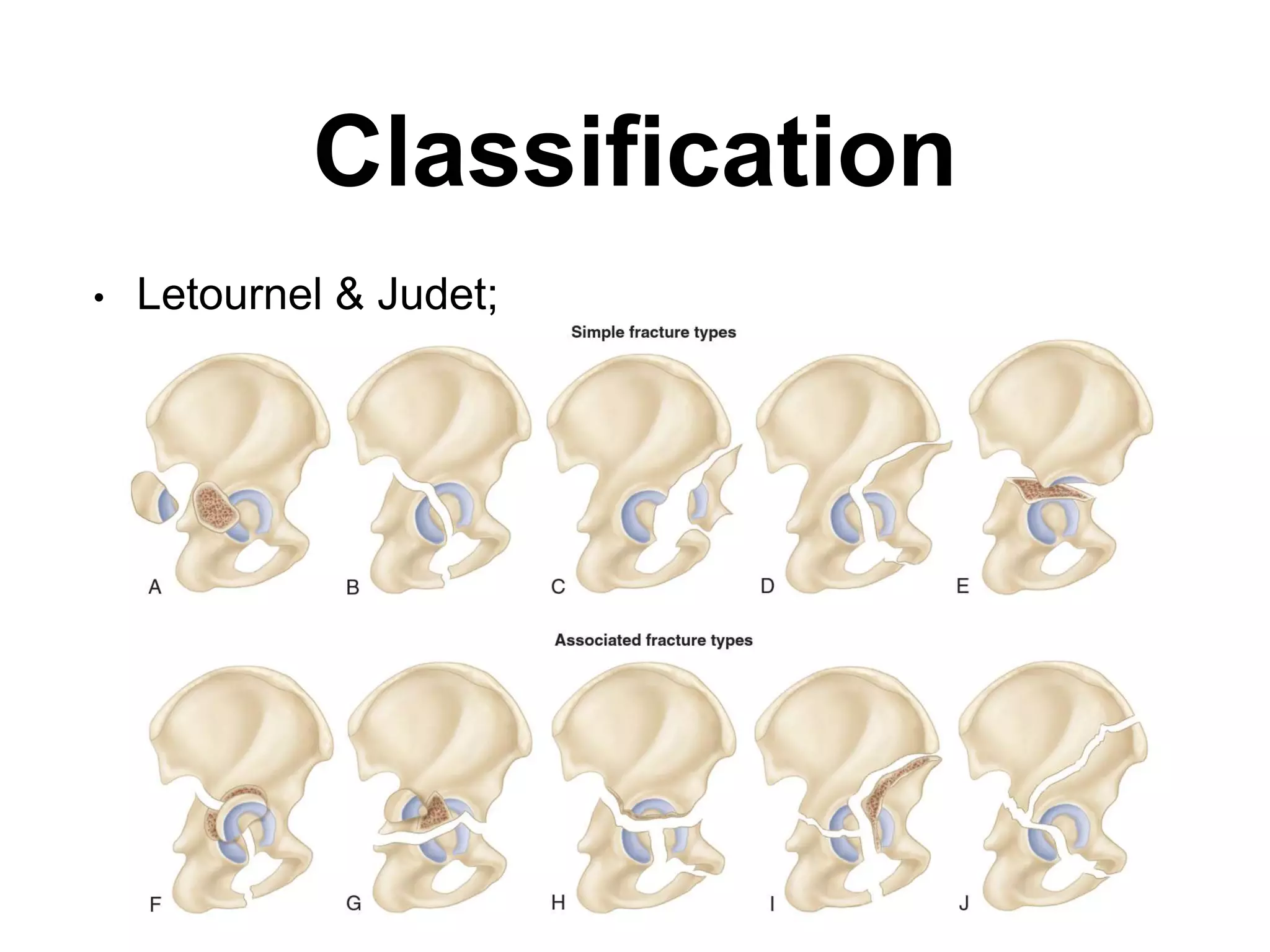
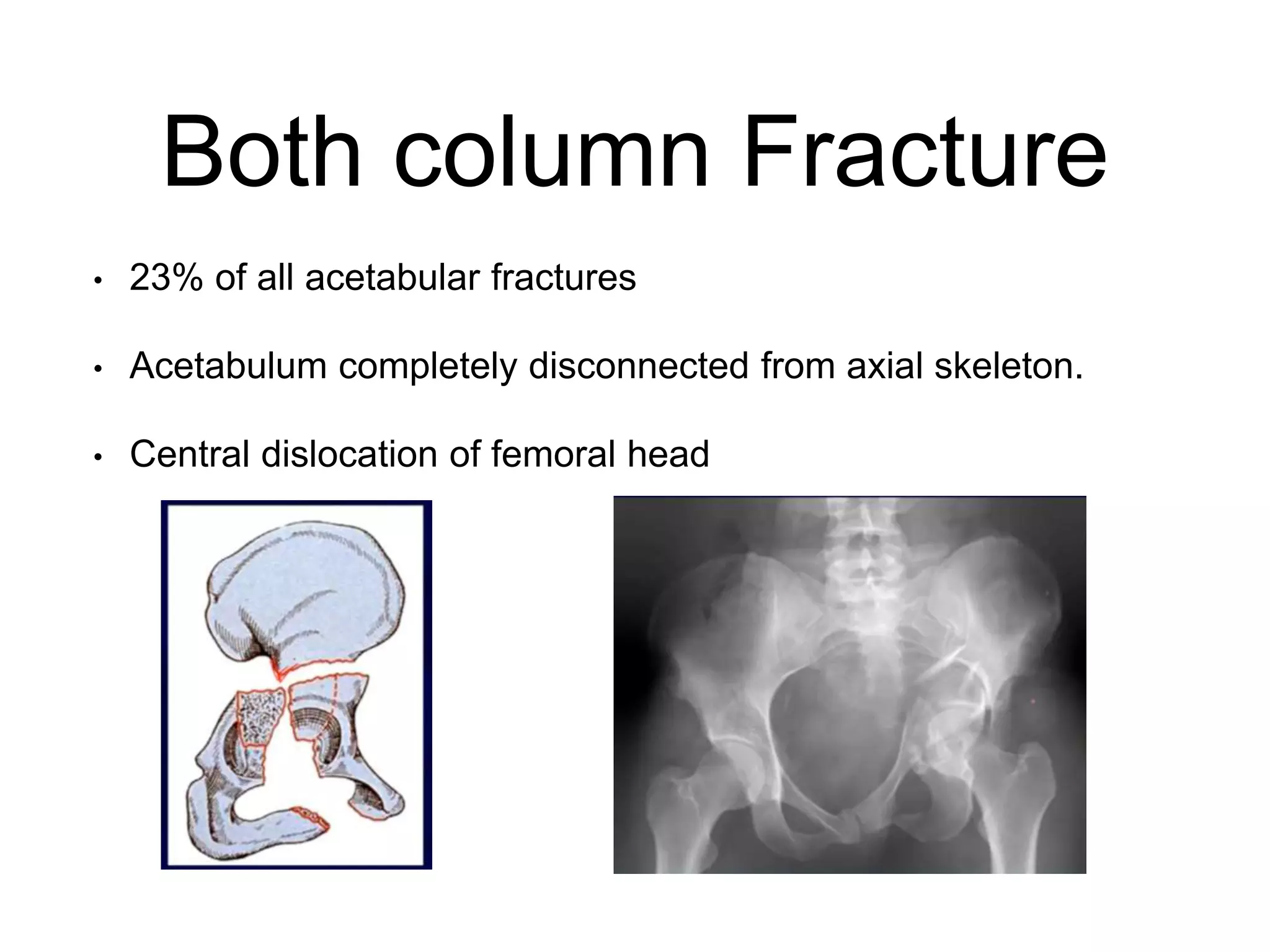
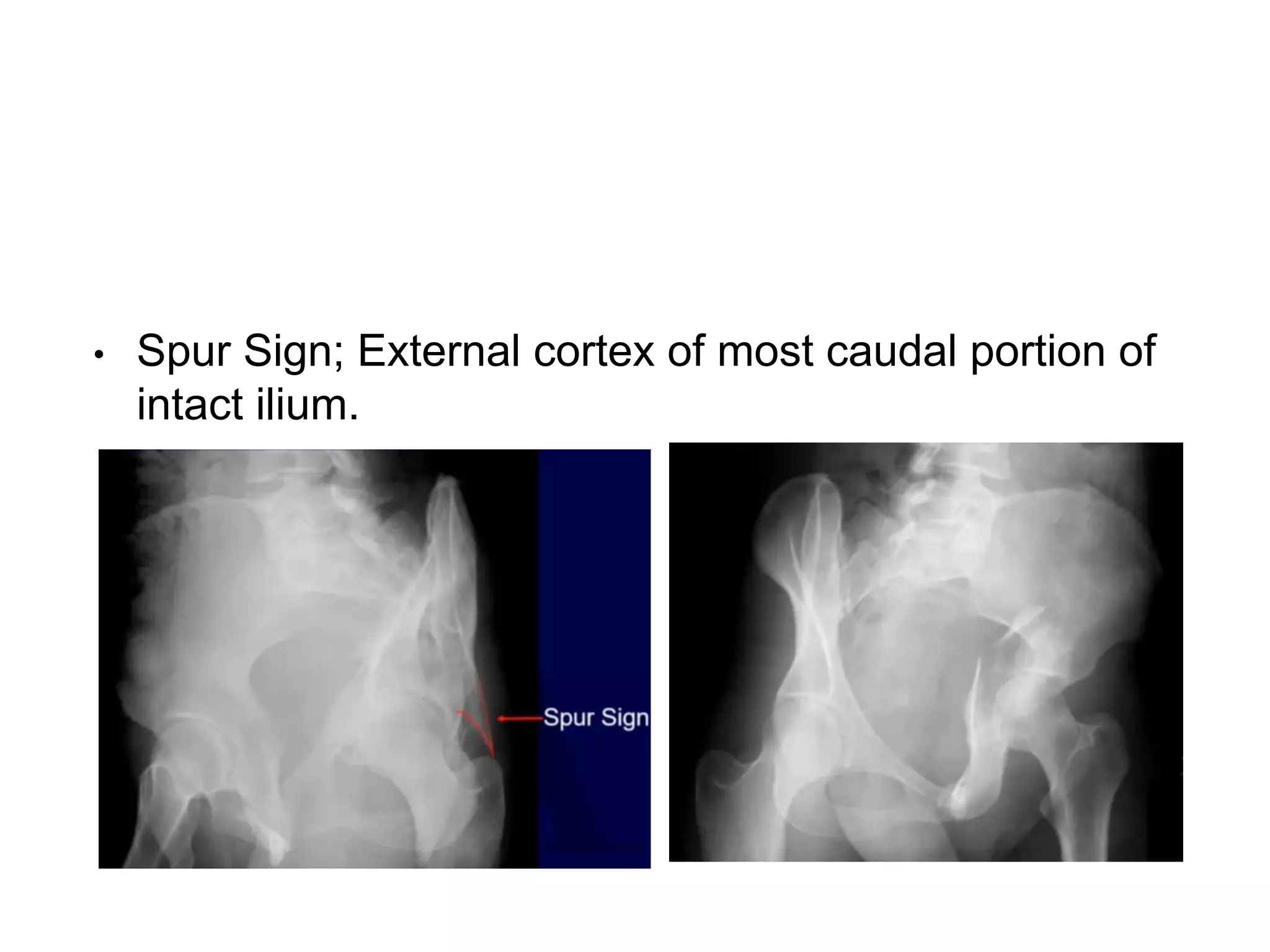
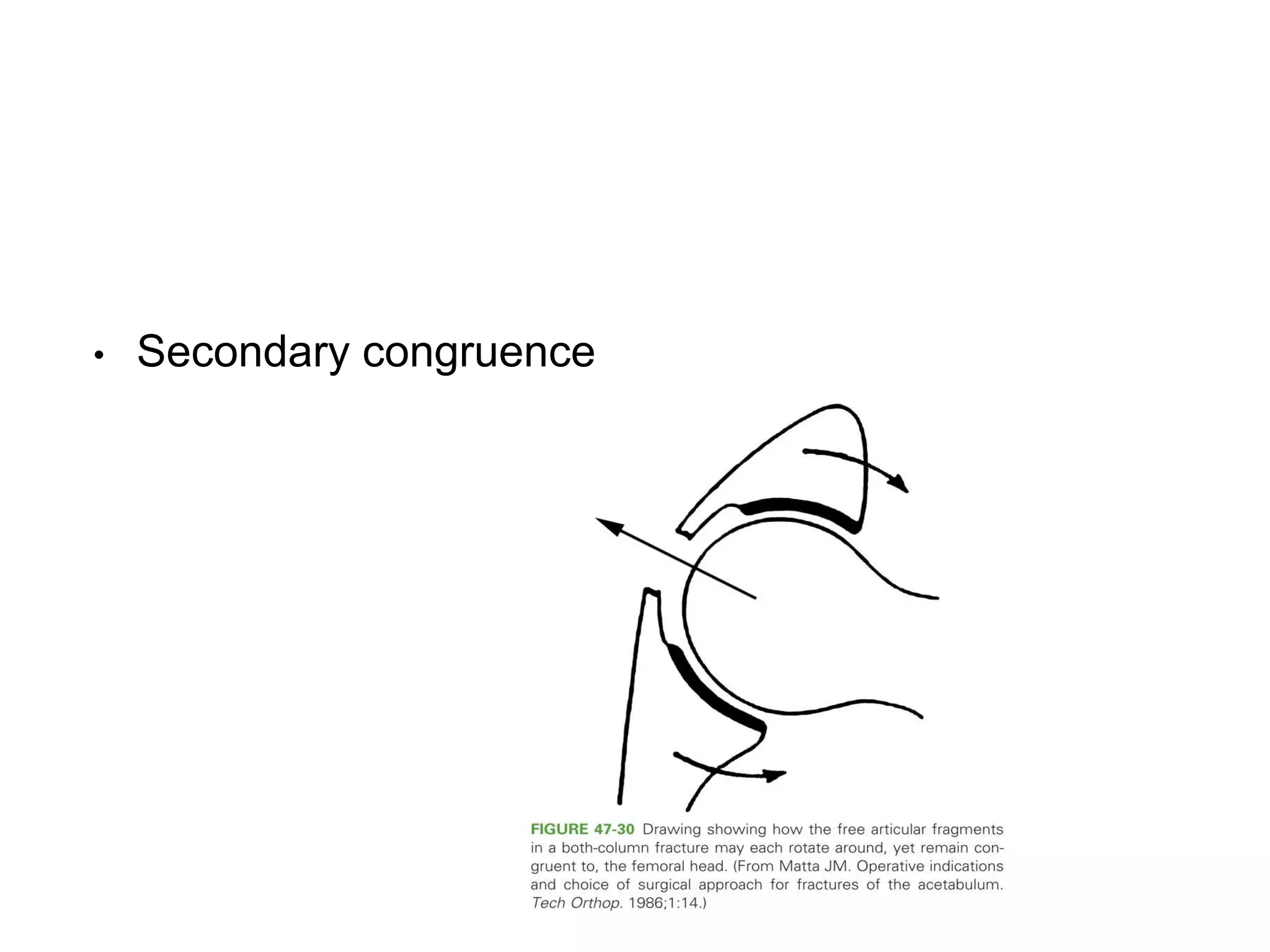
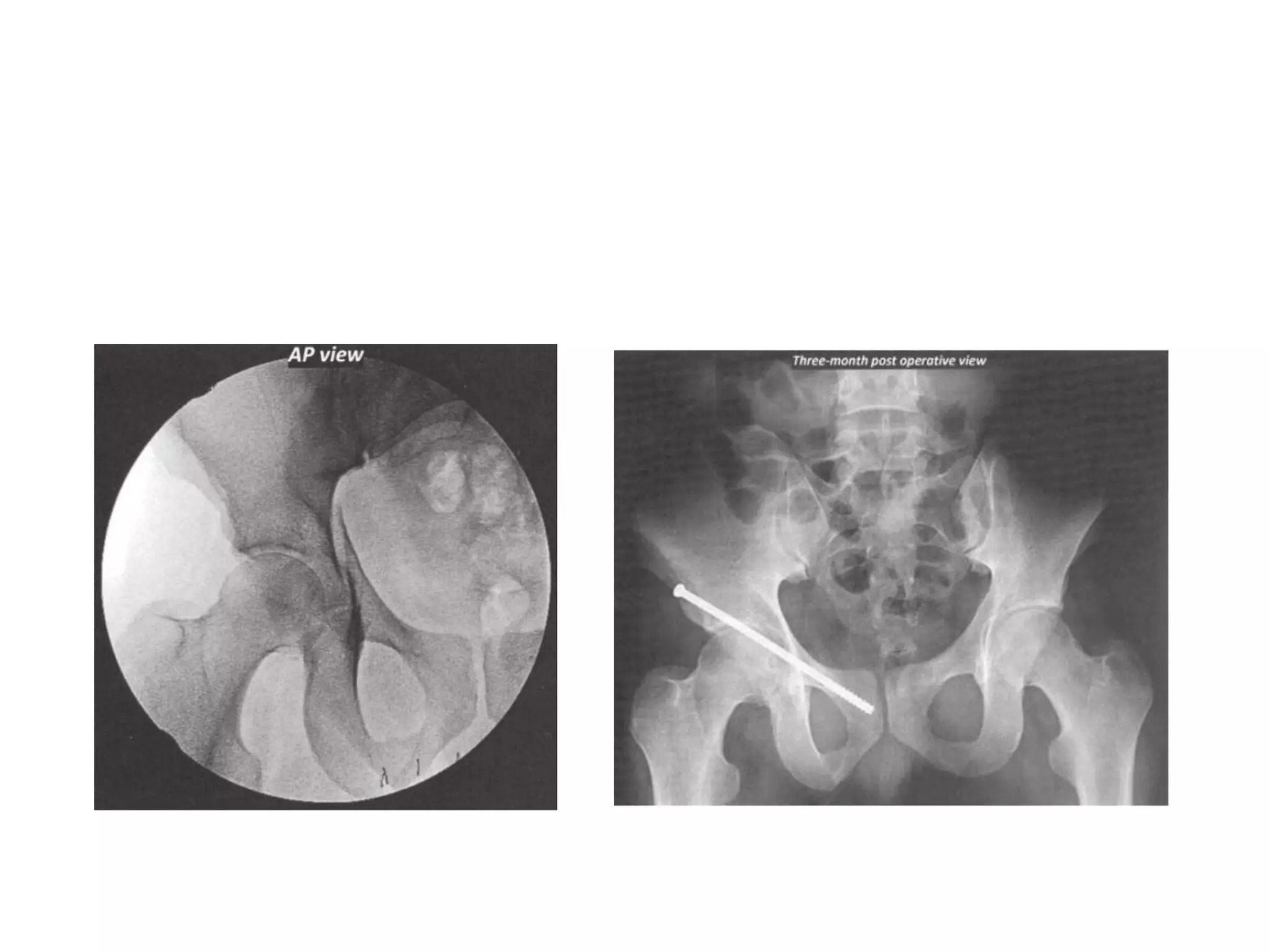
2) Surgical treatment is indicated for fractures with over 2mm of displacement or less than 45 degrees of roof arc measurement, while non-operative treatment can be used for minimally displaced fractures or those with secondary congruence.
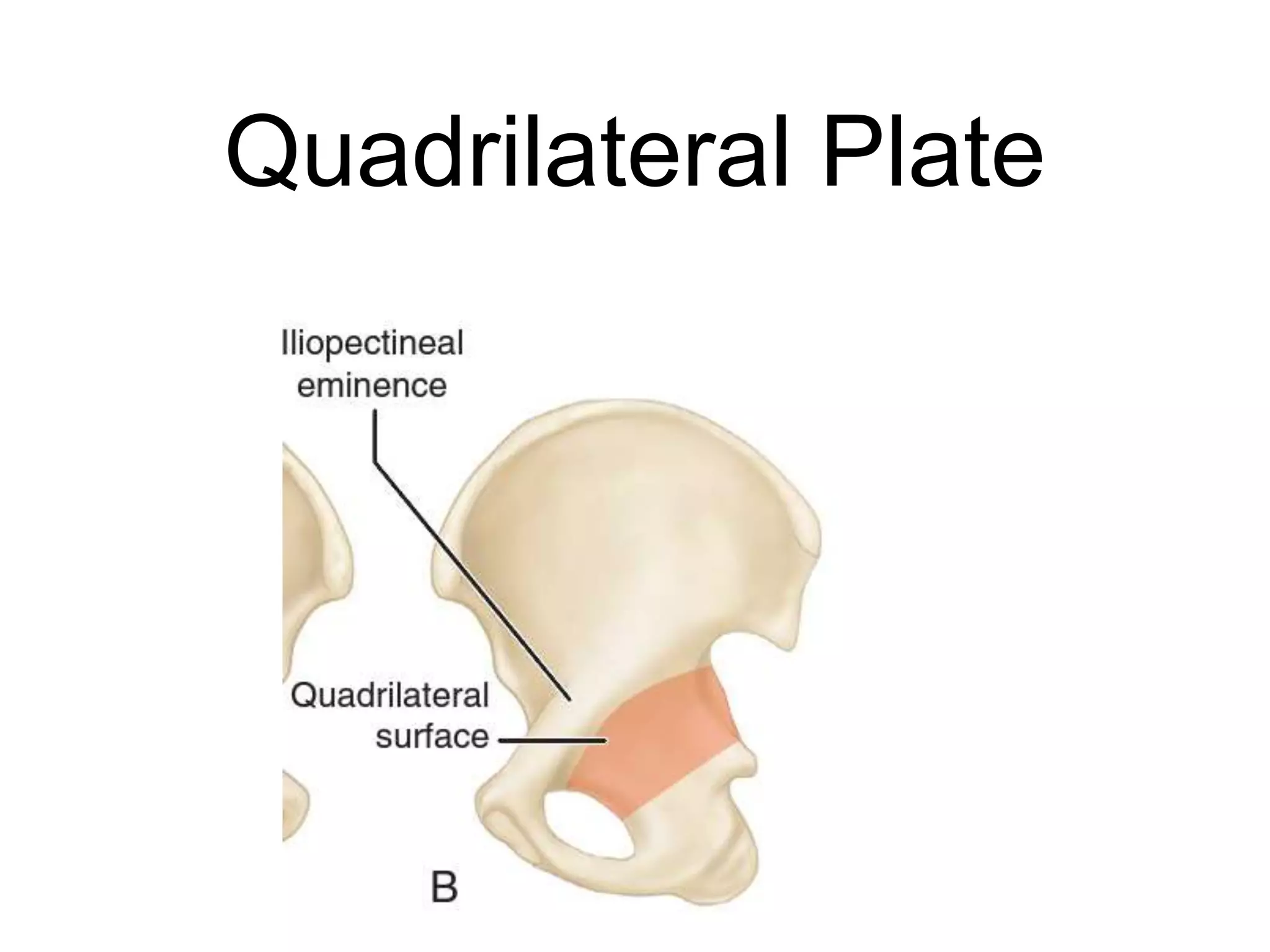
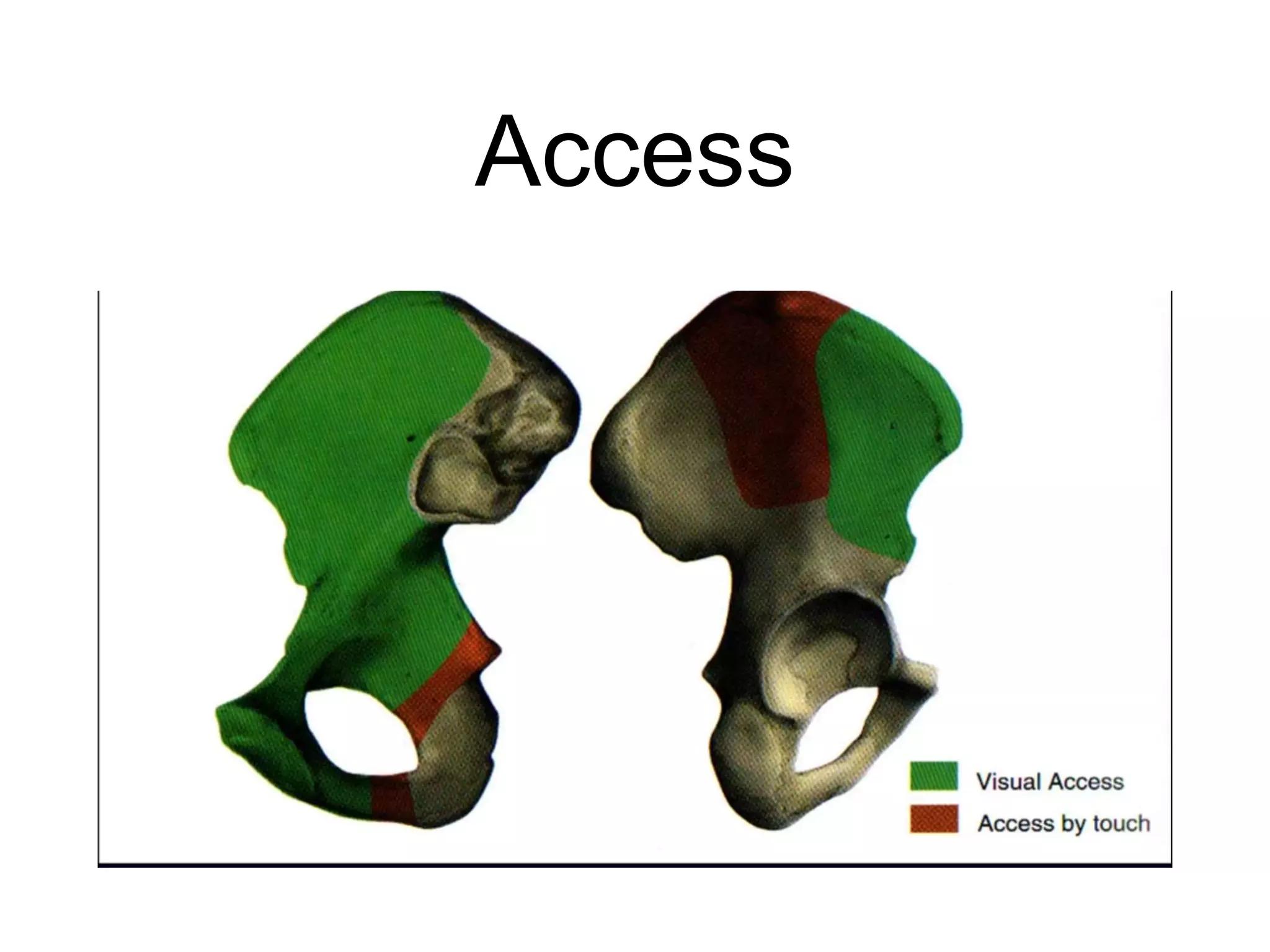
3) Surgical approaches like the modified Stoppa or Kocher-Langenbeck are selected based on the fracture pattern and aim to reduce and stabilize the displaced columns and walls with plates and screws to restore hip function.