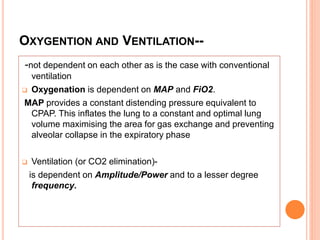
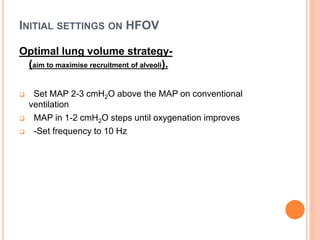
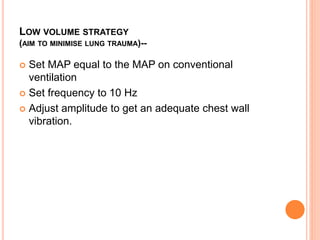
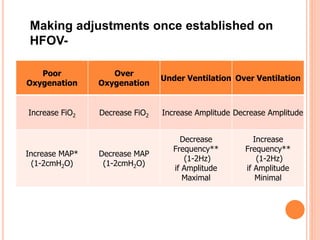
High frequency oscillatory ventilation (HFOV) uses very high rates of small pressure variations around a constant distending pressure to ventilate the lungs. It relies on diffusion and other gas exchange mechanisms rather than conventional tidal volumes. HFOV is only used as a rescue therapy for failure of conventional ventilation in term or preterm infants with conditions like PPHN or MAS. Settings are adjusted based on oxygenation and ventilation, with the goal of maximizing lung volume while avoiding overinflation and trauma.
![ A type of mechanical ventilation that uses a constant
distending pressure (mean airway pressure [MAP]) with
pressure variations oscillating around the MAP at very
high rates (up to 900 cycles per minute).
It creats small tidal volumes, often less than the dead space.
HFOV may reduce lung injury.](https://image.slidesharecdn.com/hfov-dr-170111064243/85/High-frequency-oscillatory-ventilation-Basics-2-320.jpg)
![ONLY INDICATED AS A RESCUE THERAPY-
1. Failure of conventional ventilation in the term
infant (Persistent Pulmonary Hypertension of
the Newborn [PPHN], Meconium Aspiration
Syndrome [MAS]).
2. Air leak syndromes (pneumothorax,
pulmonary interstitial emphysema [PIE])
3. Failure of conventional ventilation in the
preterm infant (severe RDS, PIE, pulmonary
hypoplasia) or to reduce barotrauma when
conventional ventilator settings are high.](https://image.slidesharecdn.com/hfov-dr-170111064243/85/High-frequency-oscillatory-ventilation-Basics-5-320.jpg)