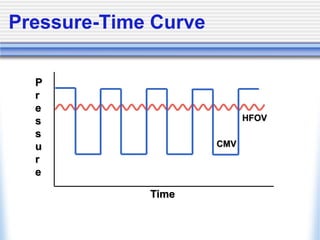
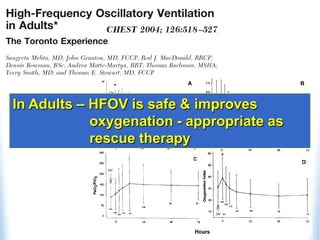
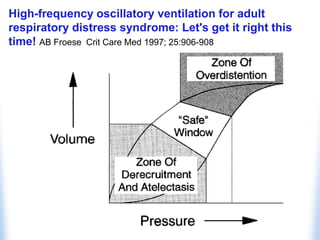
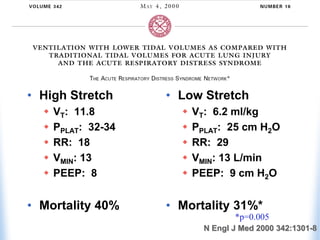
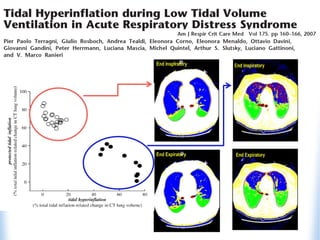
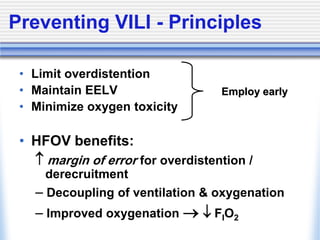
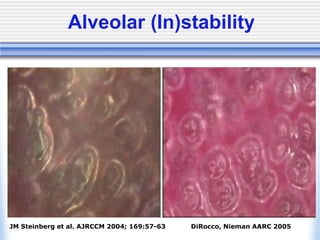
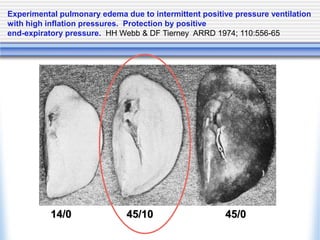
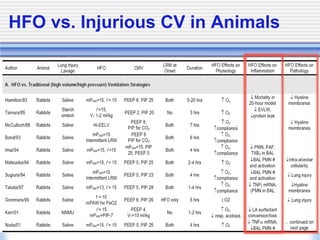
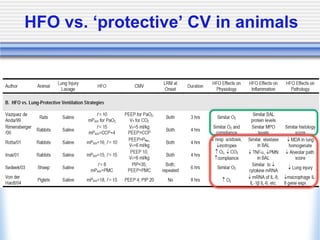
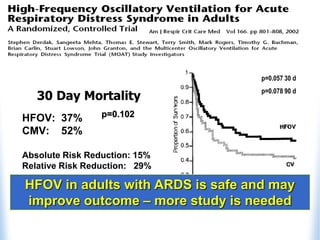
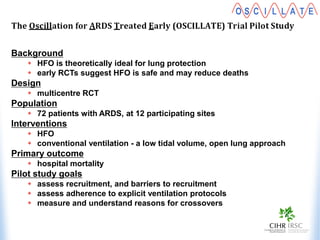
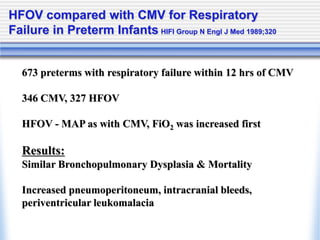
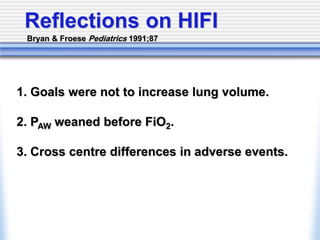
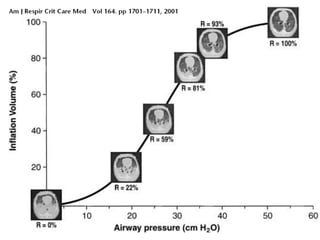
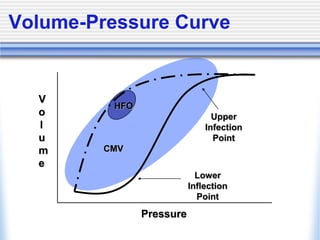
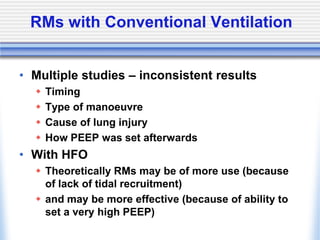
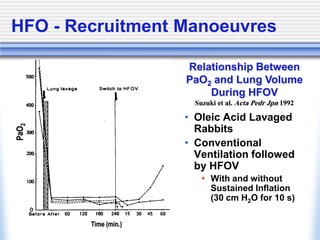
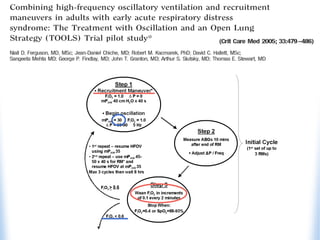
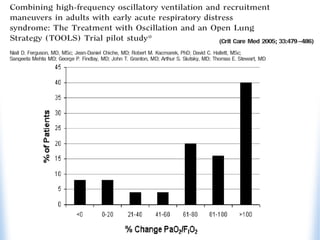
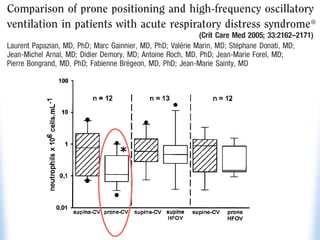
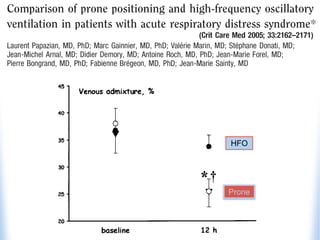
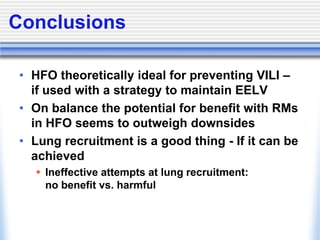
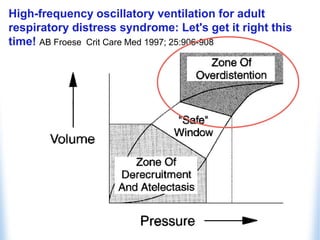
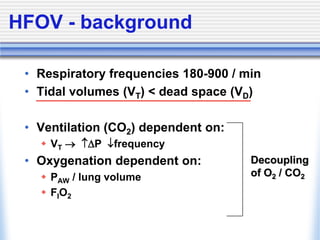
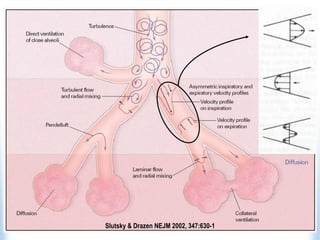
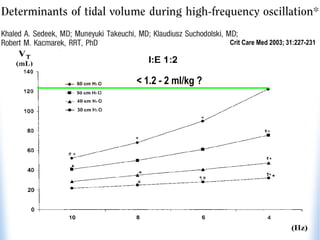
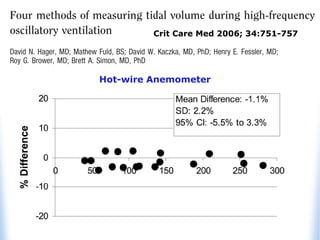
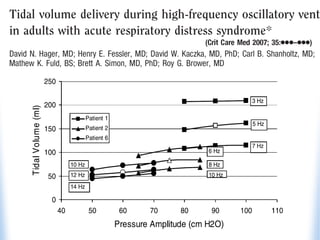
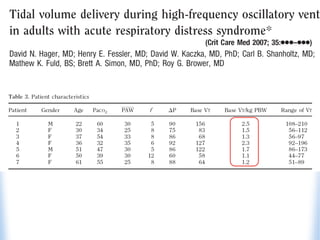
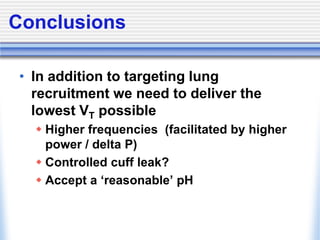
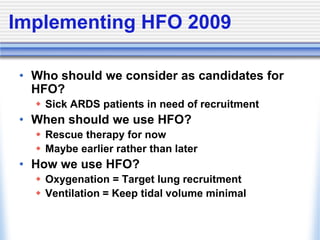
High-frequency oscillatory ventilation (HFOV) is proposed as a strategy to prevent ventilator-induced lung injury (VILI) in patients with acute respiratory distress syndrome (ARDS), with evidence indicating it may improve oxygenation and reduce mortality. The document discusses the implementation of HFOV, including candidate selection, timing, and techniques for recruitment, while emphasizing the importance of minimizing tidal volume and managing oxygenation. Further research is needed to fully understand HFOV's benefits and outcomes compared to conventional ventilation methods.