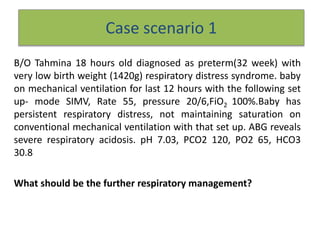
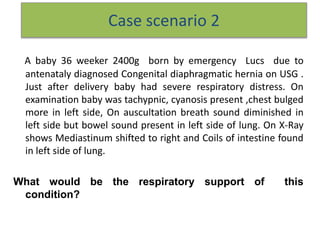
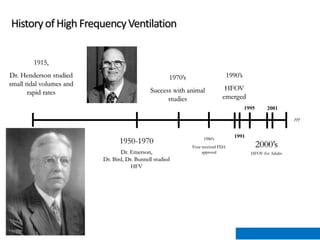
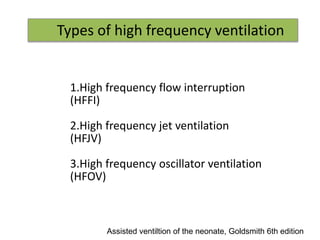
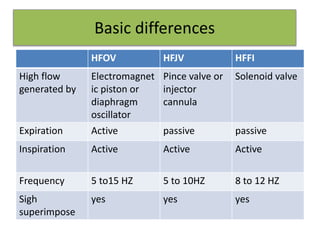
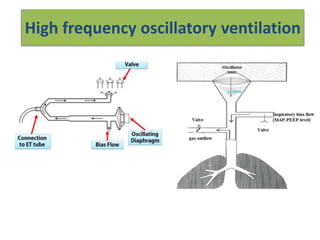
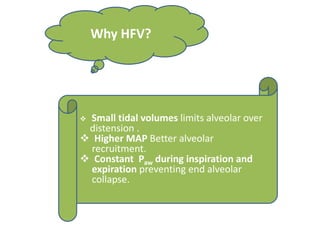
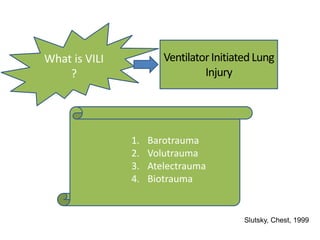
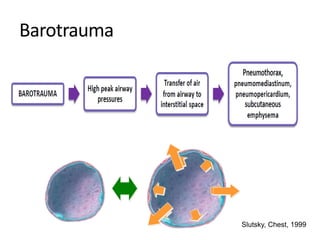
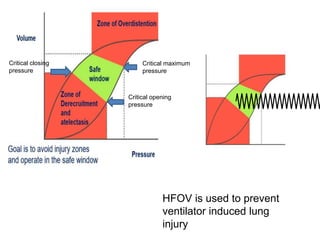
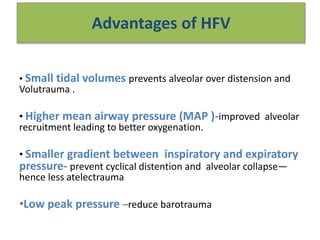
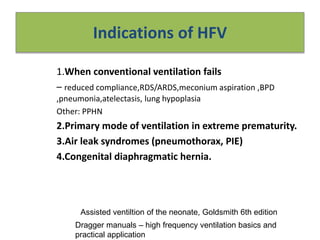
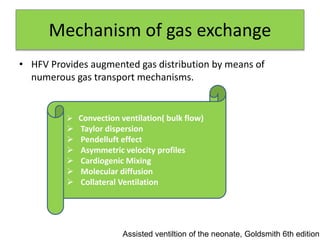
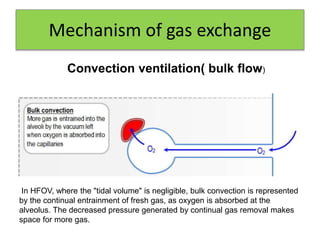
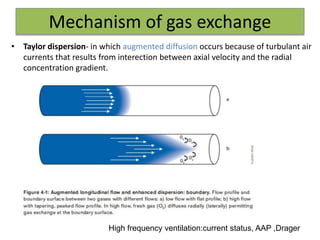
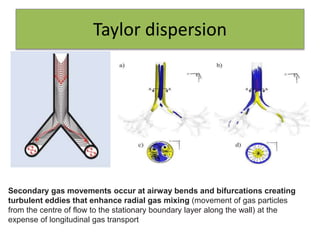
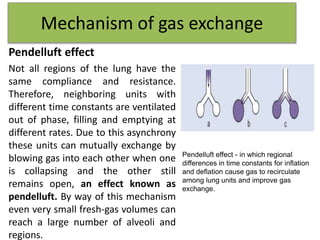
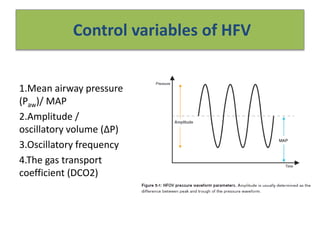
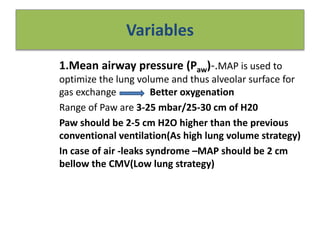
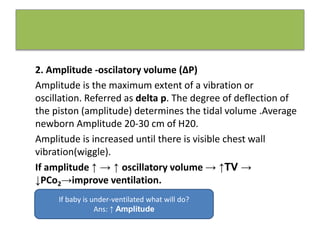
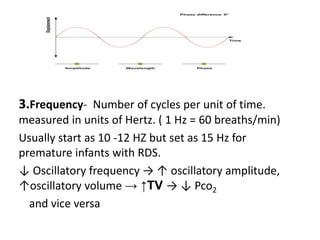
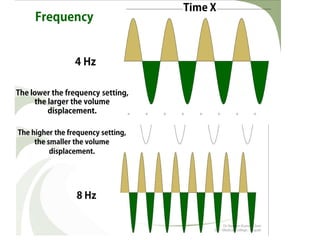
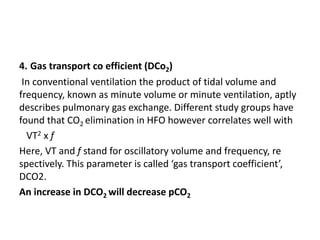
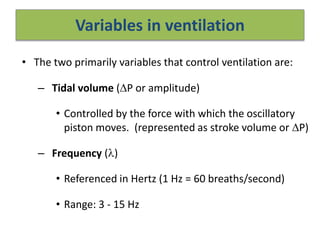
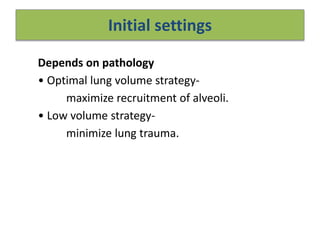
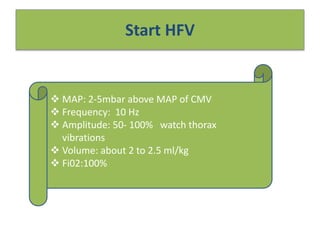
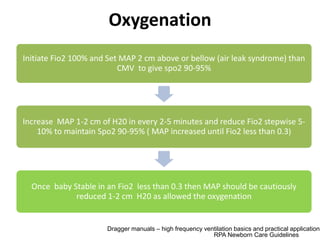
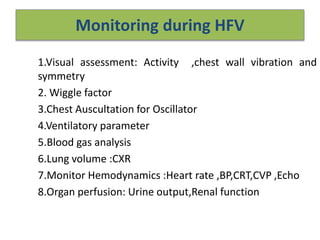
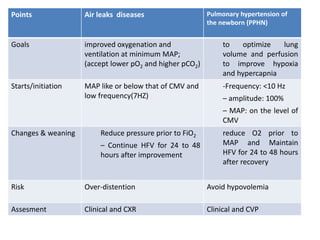
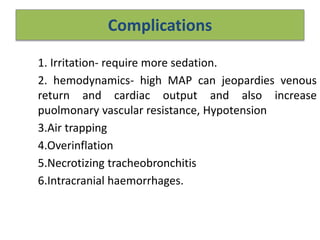
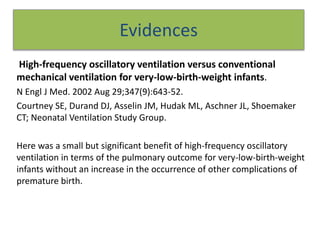
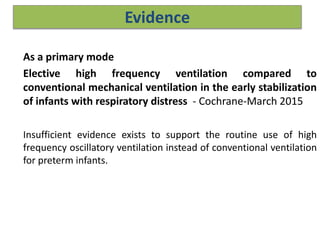
This document provides information on two case scenarios involving neonatal respiratory distress. Case 1 involves a very preterm infant with respiratory distress syndrome requiring mechanical ventilation. The infant has persistent respiratory distress and acidosis despite conventional ventilation settings. Case 2 involves an infant with congenital diaphragmatic hernia exhibiting respiratory distress at birth. The document then provides an overview of high frequency ventilation including its mechanisms, indications, settings, monitoring and complications. Evidence is presented from a randomized controlled trial showing a benefit of high frequency oscillatory ventilation over conventional ventilation for very preterm infants.