1) High frequency ventilation (HFV) uses small tidal volumes and high respiratory rates to improve gas exchange through mechanisms like molecular diffusion and pendulum flow rather than conventional alveolar ventilation.
2) HFV can be delivered through high frequency positive pressure ventilation (HFPPV), high frequency jet ventilation (HFJV), or high frequency oscillatory ventilation (HFOV).
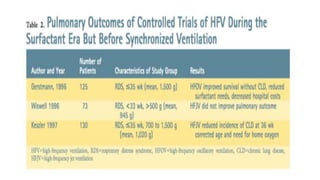
3) Evidence does not clearly support using HFV over conventional ventilation as a primary therapy for preterm infants with respiratory distress, though it may be considered as a rescue therapy when conventional ventilation fails.


![INTRODUCTION
HFV is a type of mechanical ventilation that uses a constant distending
pressure (mean airway pressure [MAP]) with pressure variations
oscillating around the MAP at very high rates
This creates small tidal volumes, often less than the dead space. HFOV
relies on alternative mechanisms of gas exchange such as molecular
diffusion, Taylor dispersion, turbulence, asymmetric velocity profiles,
Pendelluft, cardiogenic mixing and collateral ventilation](https://image.slidesharecdn.com/hfvneonates-170214164809/85/HIGH-FREQUENCY-VENTILATION-NEONATES-3-320.jpg)

















![USES
1. failure of conventional ventilation in the term infant (Persistent
Pulmonary Hypertension of the Newborn [PPHN], Meconium
Aspiration Syndrome [MAS]).4,5
2. Air leak syndromes (pneumothorax, pulmonary interstitial
emphysema [PIE])7
3. Failure of conventional ventilation in the preterm infant (severe
RDS, PIE, pulmonary hypoplasia) or to reduce barotrauma when
conventional ventilator settings are high.
4. Lung hypoplasia syndromes](https://image.slidesharecdn.com/hfvneonates-170214164809/85/HIGH-FREQUENCY-VENTILATION-NEONATES-22-320.jpg)