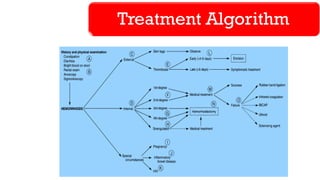
The document provides a comprehensive overview of lower gastrointestinal (GI) hemorrhage due to hemorrhoids, including their causes, classifications, clinical features, investigations, complications, and treatment options. It details the etiopathogenesis of hemorrhoids, the diagnostic process, and various nonoperative and operative treatment methods. Specific case studies exemplify the presentation and diagnosis of hemorrhoids, highlighting both internal and external forms.