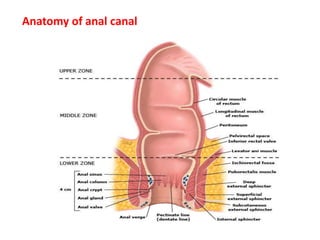
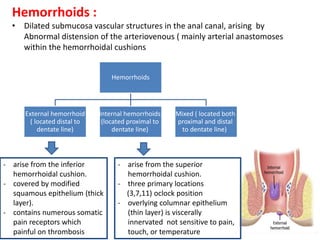
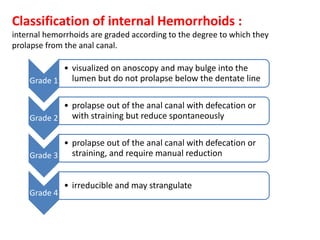
This document discusses hemorrhoids, including their anatomy, classification, risk factors, pathogenesis, clinical features, diagnosis, differential diagnosis, and management. Some key points:
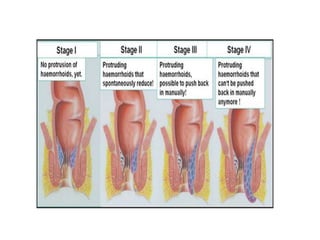
- Hemorrhoids are dilated submucosa vascular structures in the anal canal that can be internal, external, or mixed. Internal hemorrhoids are further classified into four grades based on degree of prolapse.
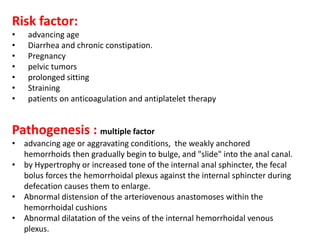
- Risk factors include advancing age, diarrhea/constipation, pregnancy, prolonged sitting, and straining. Pathogenesis involves weakening of supporting tissues and increased pressure on hemorrhoids during defecation.
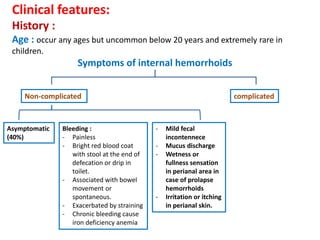
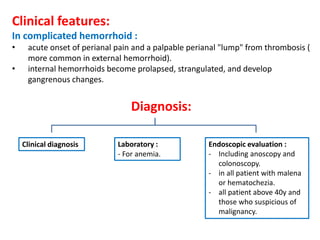
- Clinical features depend on whether hemorrhoids are complicated or uncomplicated, and may include bleeding, pain,