This document provides information on haemorrhoids (also known as hemorrhoids), including:
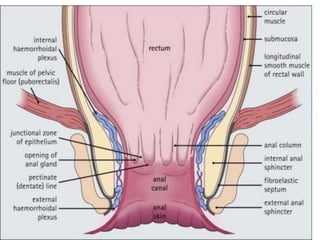
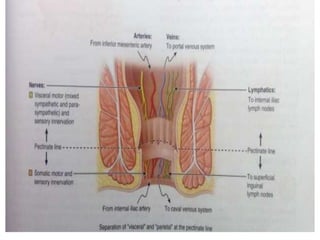
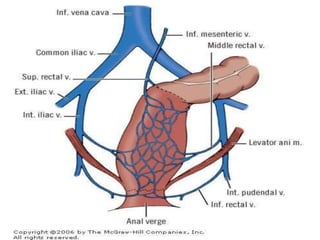
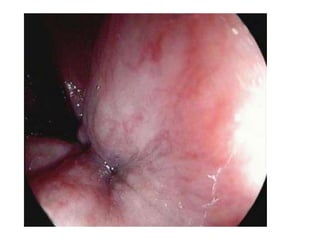
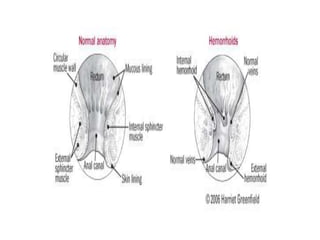
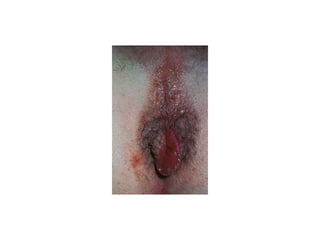
- Anatomy of the anal canal and haemorrhoidal tissue
- Epidemiology of symptomatic haemorrhoids, affecting around 4.4% of the global population
- Common causes like straining, pregnancy, obesity, and familial tendency
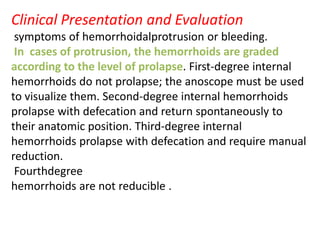
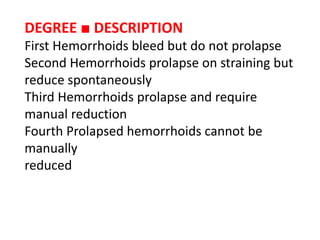
- Grading of internal haemorrhoids from first to fourth degree based on degree of prolapse
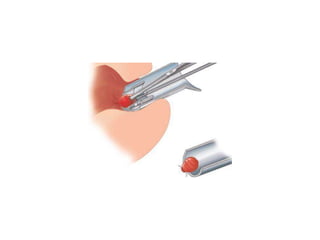
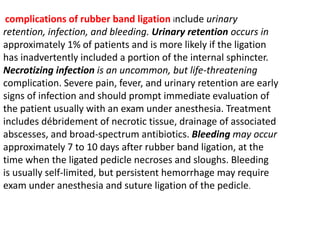
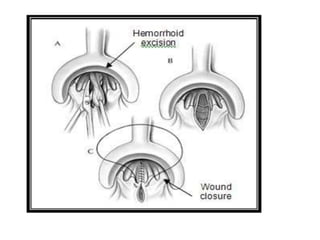
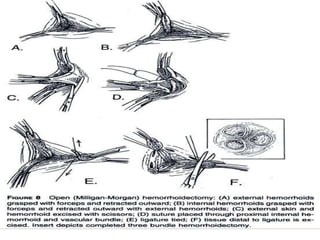
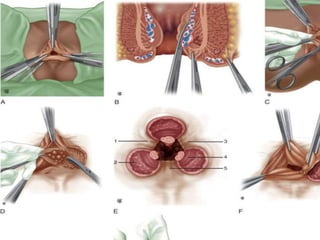
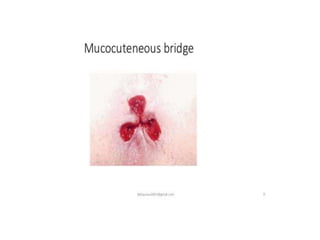
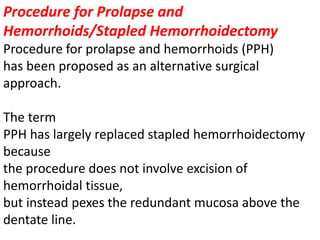
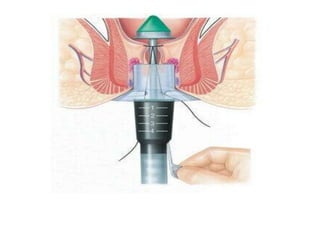
- Treatment options like rubber band ligation, sclerotherapy, excisional or stapled haemorrhoidectomy depending on severity