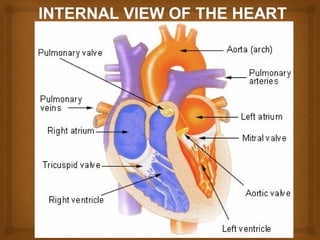
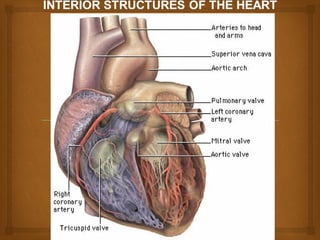
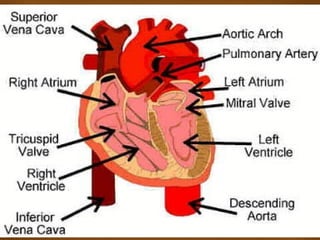
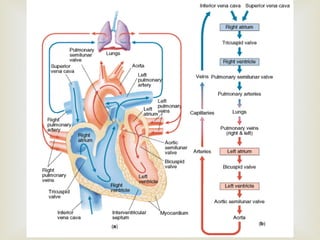
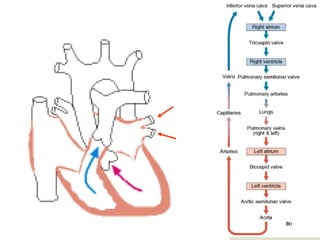
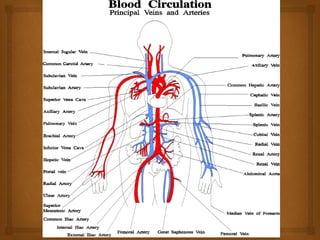
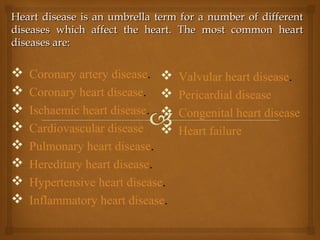
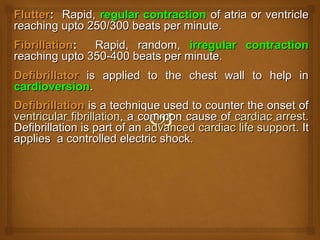
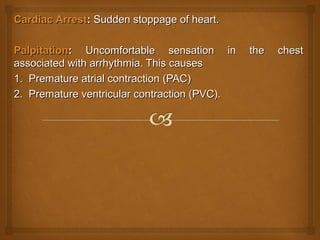
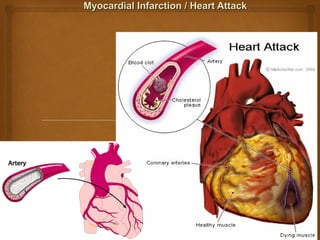
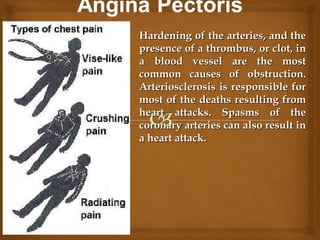
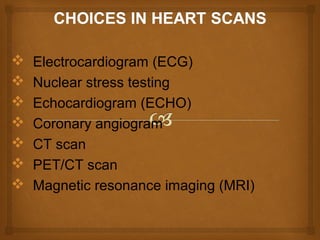
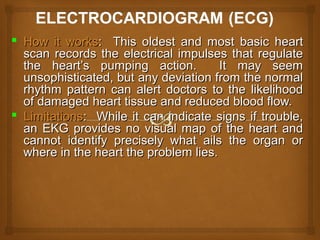
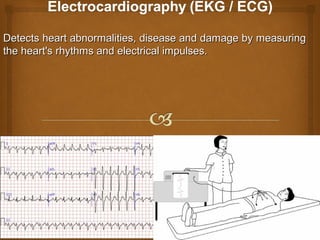
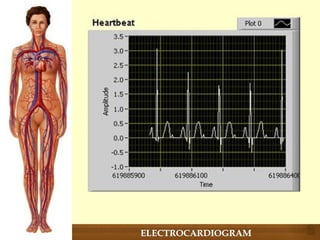
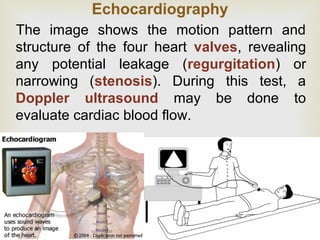
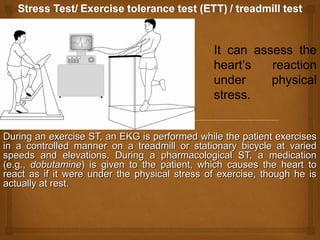
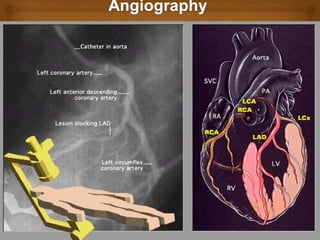
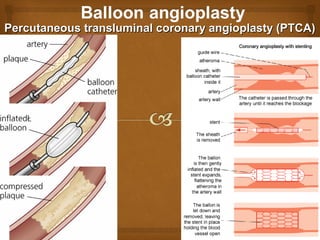
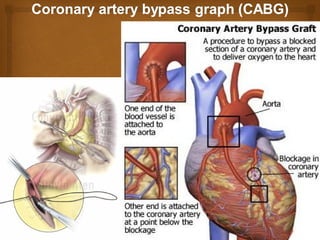
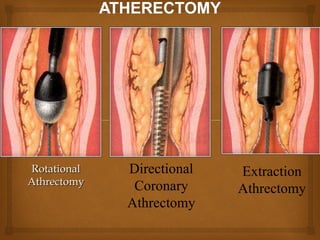
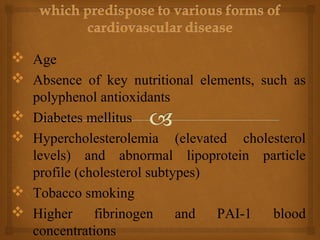
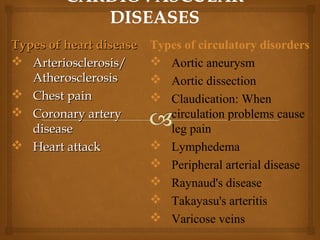
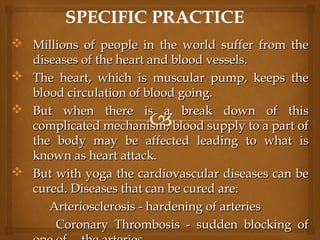
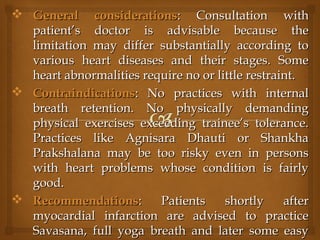
The heart is divided into four chambers by septa and valves. The document discusses the anatomy and function of the heart and blood vessels. It then describes various heart diseases and conditions such as coronary artery disease, heart failure, arrhythmias, and methods used to diagnose and treat heart disease.