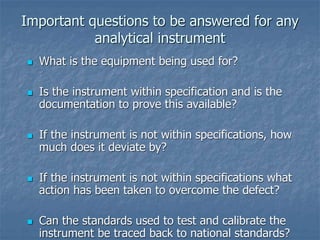
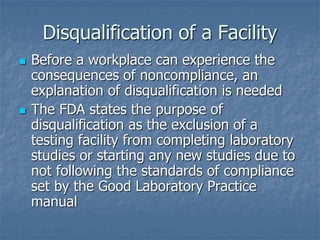
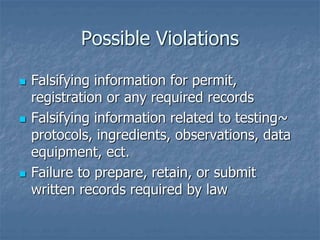
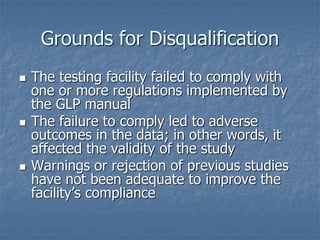
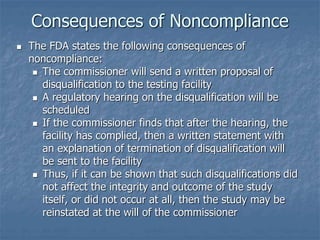
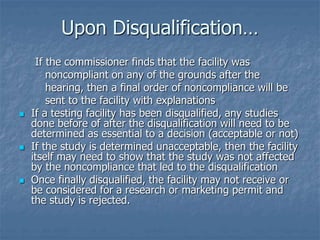
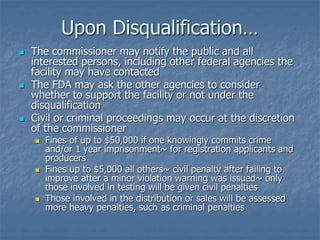
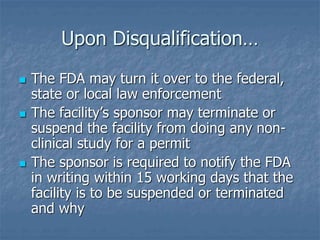
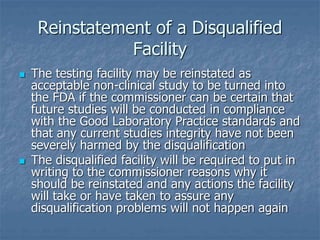
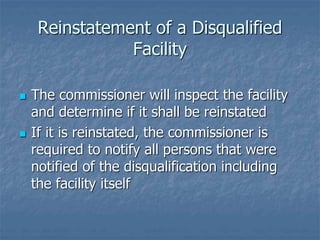
The document discusses Good Laboratory Practices (GLP), which are regulations created by the FDA in 1978 that provide a framework for conducting laboratory studies. GLP was established in response to cases of poor laboratory practices including fraudulent activities and inaccurate reporting of results. The objectives of GLP are to ensure data submitted accurately reflects study results and is traceable. Laboratories must comply with requirements around facilities, equipment, recordkeeping, personnel qualifications and standard operating procedures to adhere to GLP. Noncompliance can result in disqualification and civil or criminal penalties for the laboratory.