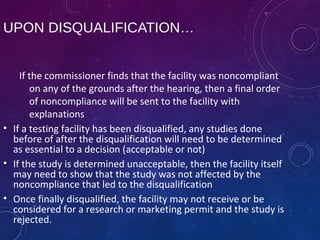
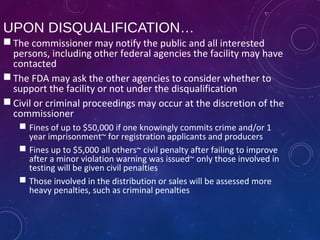
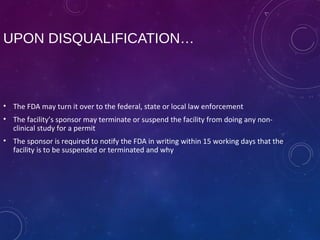
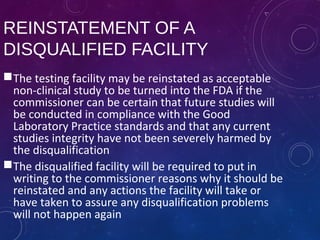
This document provides an overview of Good Laboratory Practices (GLP). It states that GLP is an FDA regulation that establishes a framework for conducting laboratory studies. The document discusses the history of GLP, including how it originated in the US in 1978 in response to cases of poor laboratory practices. It describes the objectives and mission of GLP to ensure data integrity and traceability. Key aspects of GLP like standard operating procedures, record keeping, and facility certification are summarized. Consequences of noncompliance, such as disqualification and inability to conduct studies, are also outlined.