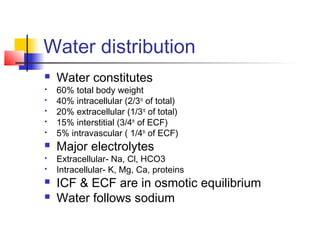
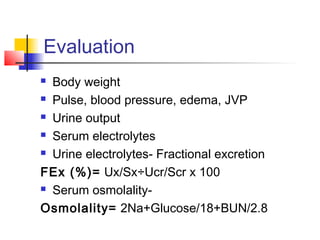
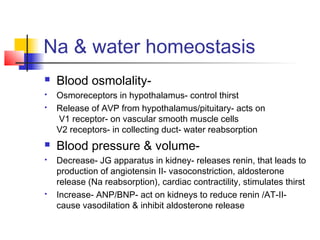
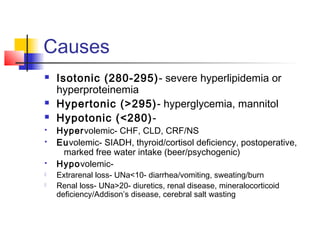
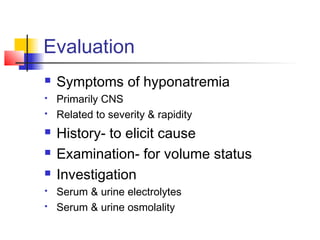
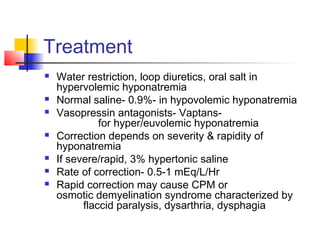
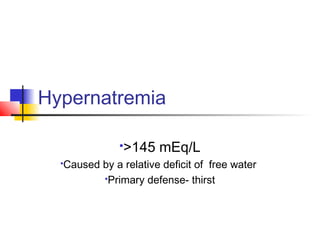
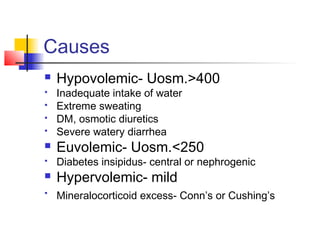
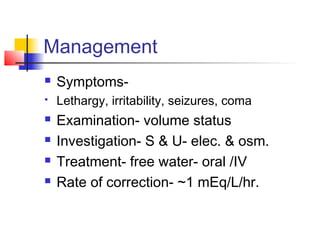
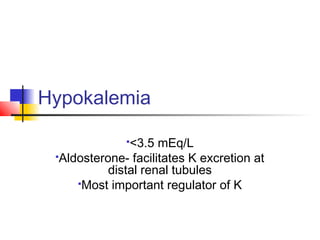
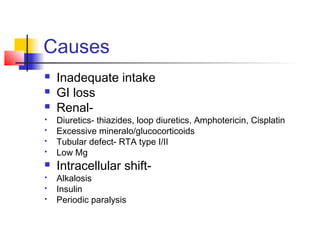
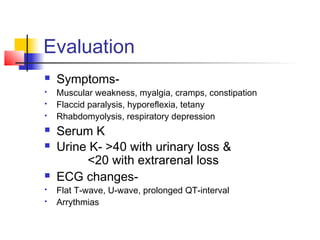
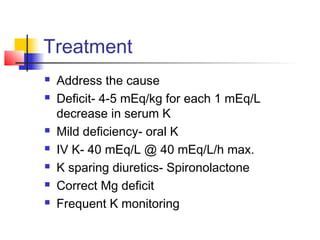
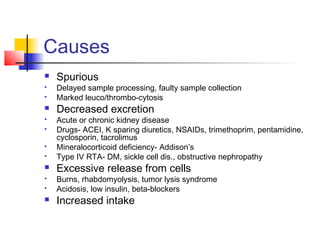
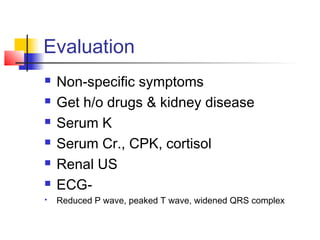
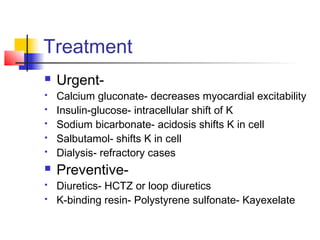
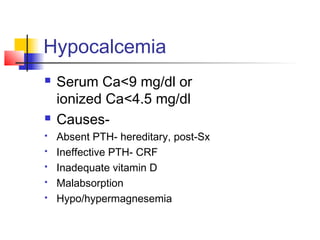
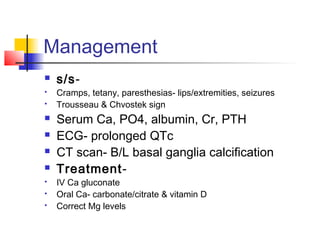
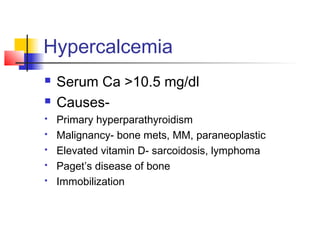
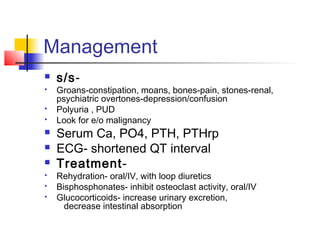
This document discusses fluid and electrolyte imbalances. It covers water distribution in the body, the roles of major electrolytes like sodium, potassium, calcium, and their regulation. Causes, evaluation, and treatment approaches for various electrolyte abnormalities like hyponatremia, hypernatremia, hypokalemia, hyperkalemia, hypocalcemia, and hypercalcemia are summarized. Evaluation involves assessing symptoms, medical history, examination, and lab tests of serum and urine electrolytes and osmolality. Management depends on the specific imbalance and aim of correcting underlying causes and abnormal electrolyte levels.