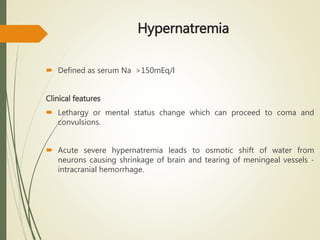
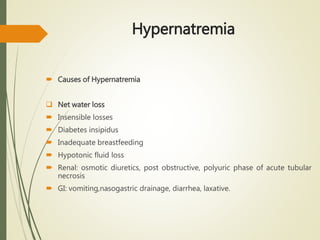
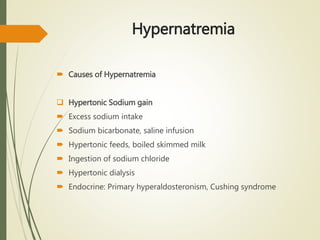
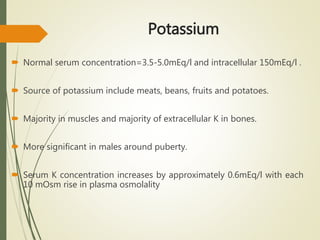
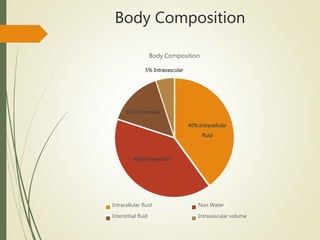
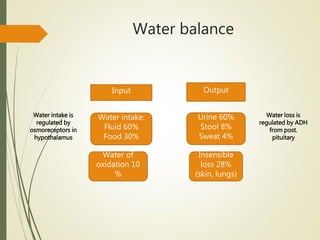
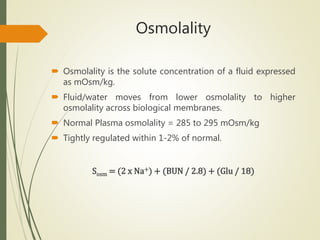
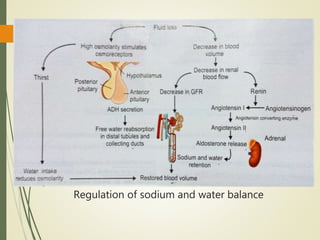
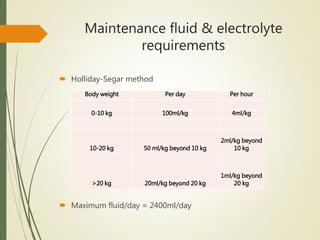
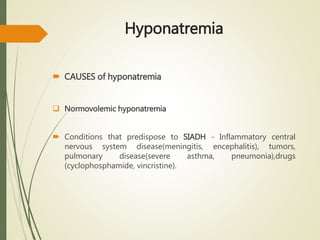
This document discusses electrolyte abnormalities in children. It provides information on the composition of body fluids, water balance, and maintenance fluid and electrolyte requirements in children. It then focuses on abnormalities in sodium, potassium, and other electrolytes. For each abnormality, it describes the causes, clinical features, evaluation, and treatment approaches. It emphasizes the importance of determining the underlying cause and correcting abnormalities slowly and carefully to avoid complications.

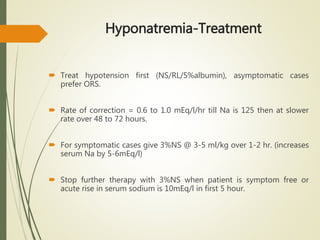
![Hyponatremia-Treatment
Determine whether hyponatremia is acute(<24 hr) or chronic(>48hr),
symptomatic/asymptomatic.
Evaluate the volume status (hypervolemia, euvolemia, hypovolemia).
Sodium deficit (meq) = 0.6*Body wt(kg) * [desired Na – observed Na]](https://image.slidesharecdn.com/electrolytesabnormalities-160302112007/85/Electrolytes-abnormalities-19-320.jpg)
![Hyponatremia-Treatment
Rise in serum Na can be estimated by Adrogue Madias formula-
Δ 𝑁𝑎 =
𝐼𝑛𝑓𝑢𝑠𝑎𝑡𝑒 𝑁𝑎 + 𝐼𝑛𝑓𝑢𝑠𝑎𝑡𝑒 𝐾 −𝑆𝑒𝑟𝑢𝑚 𝑁𝑎
[𝑇𝐵𝑊+1]
Δ[Na]= expected change in serum sodium/L of fluid given
TBW= total body water is 0.6*Body wt (kg)](https://image.slidesharecdn.com/electrolytesabnormalities-160302112007/85/Electrolytes-abnormalities-21-320.jpg)