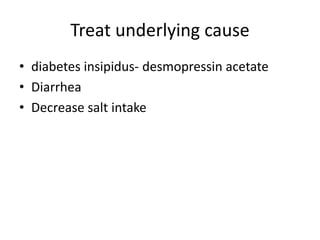
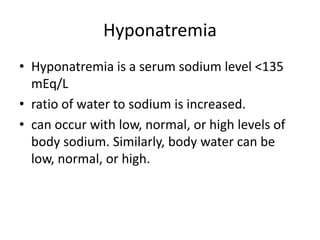
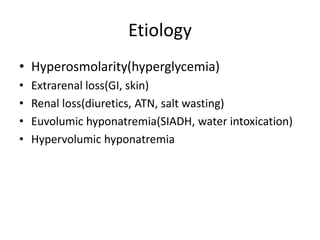
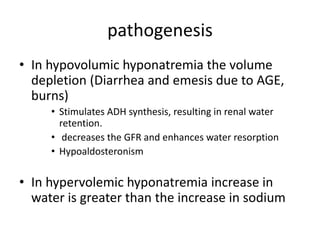
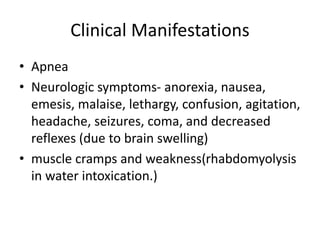
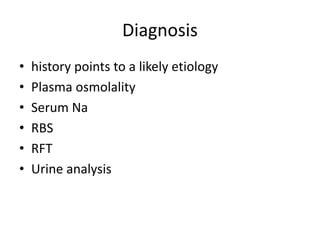
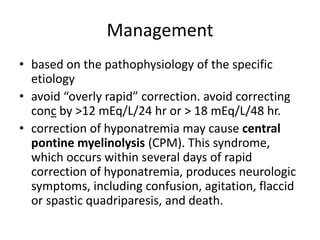
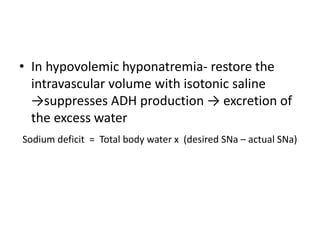
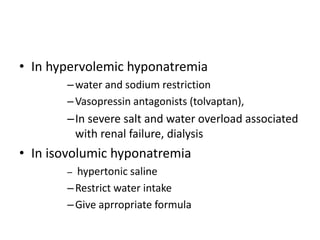
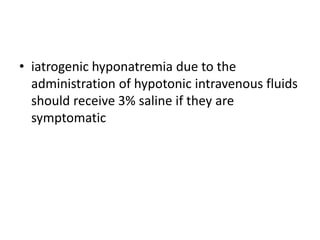
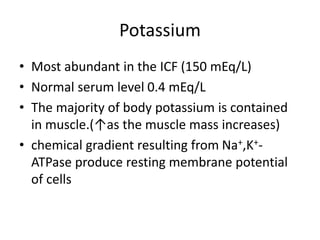
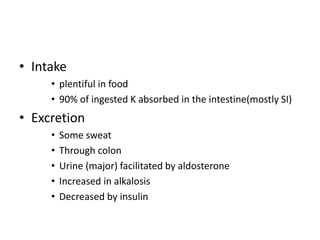
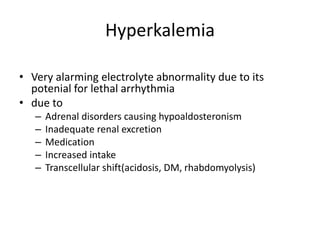
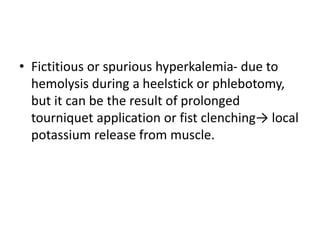
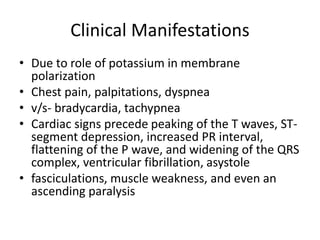
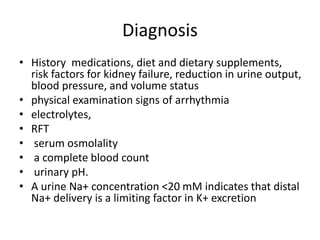
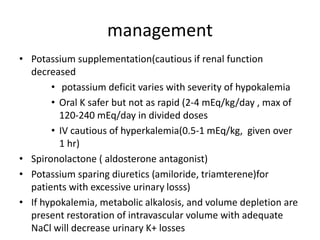
This document provides an overview of electrolyte imbalances, particularly focusing on sodium and potassium disorders like hypernatremia and hyponatremia, along with their causes, clinical manifestations, diagnosis, and management strategies. Key points include the mechanisms underlying these imbalances, the potential complications from rapid corrections, and specific treatment recommendations based on the underlying causes. Additionally, it discusses the roles of sodium and potassium in the body and the importance of monitoring patients for arrhythmias and neurological symptoms associated with these electrolyte disturbances.
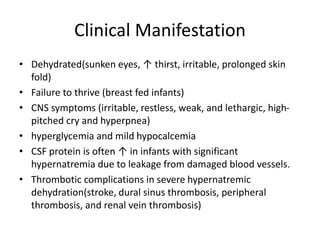
![Water deficit
• The sodium concentration of the deficit replacement
fluid, the rate of fluid administration, and the
presence of continued water losses determine the
rate of decrease of the sodium concentration. The
following formula is often cited for calculating the
water deficit:
water deficit= body weight × 0.6(1-[145/current Na])](https://image.slidesharecdn.com/electrolyteimbalanceseminar-240708185727-ad73d5f4/85/Common-electrolyte-Imbalance-in-pediatrics-11-320.jpg)
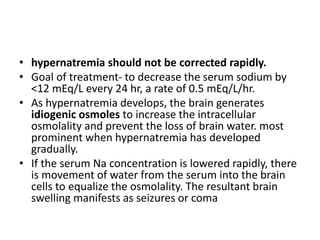
![• With sodium overload, hypernatremia is
corrected with sodium-free intravenous fluid (5%
dextrose in water [D5W]).
• When hypernatremia is due to sodium
intoxication peritoneal dialysis allows for removal
of the excess sodium.
• Hyperglycemia from hypernatremia is not treated
with insulin because the acute decrease in
glucose may precipitate cerebral edema by
lowering plasma osmolality](https://image.slidesharecdn.com/electrolyteimbalanceseminar-240708185727-ad73d5f4/85/Common-electrolyte-Imbalance-in-pediatrics-13-320.jpg)