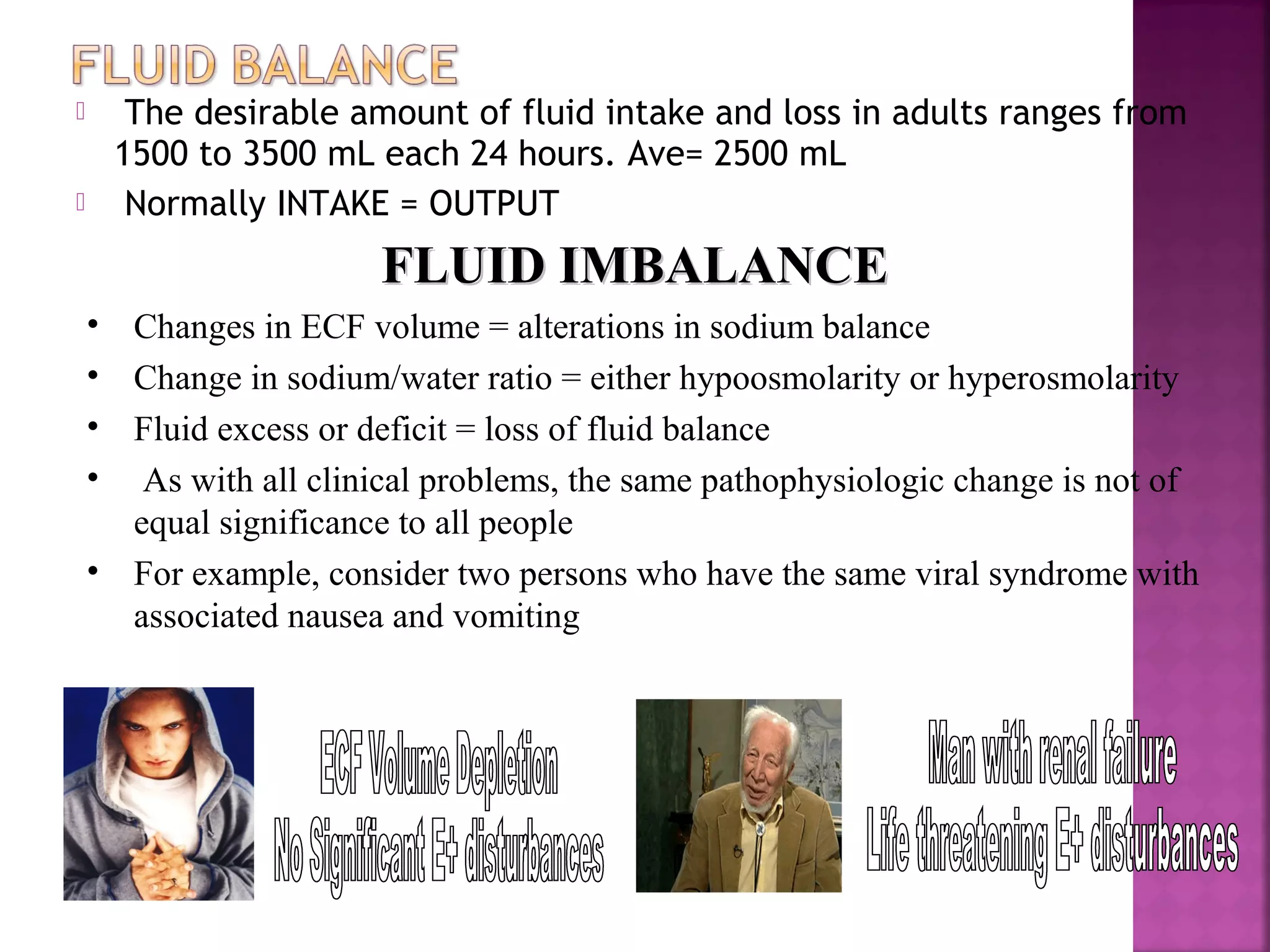
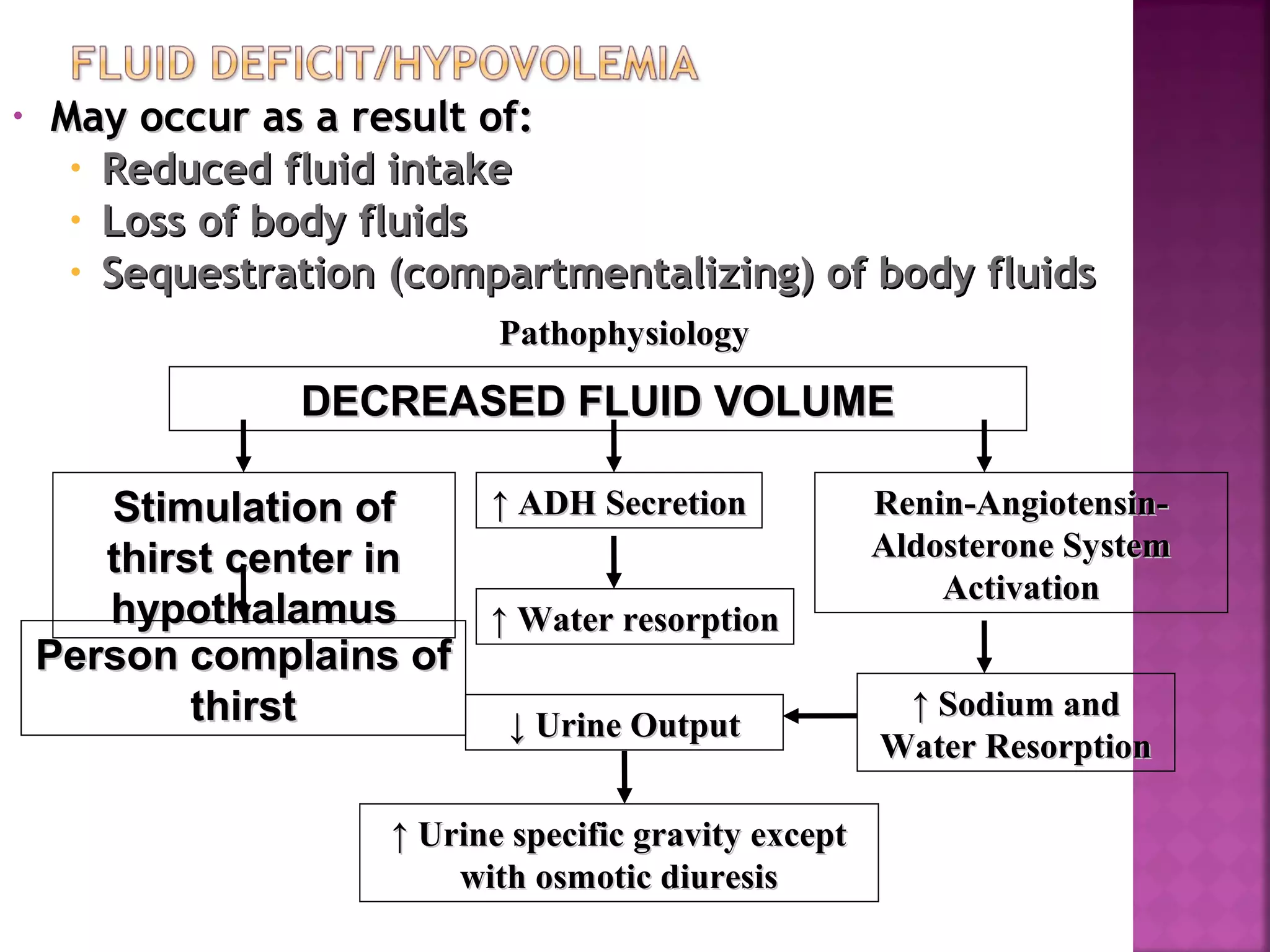
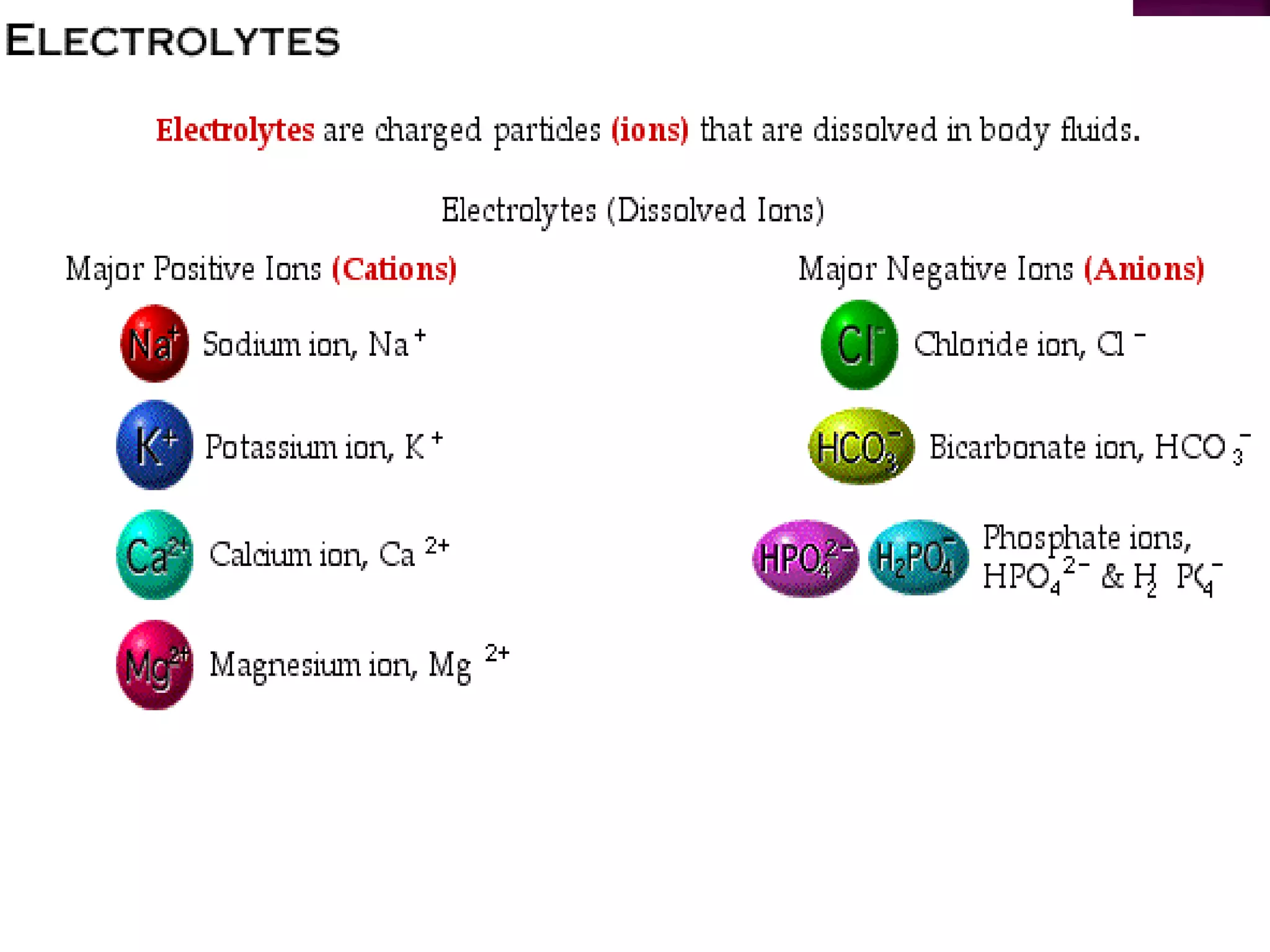
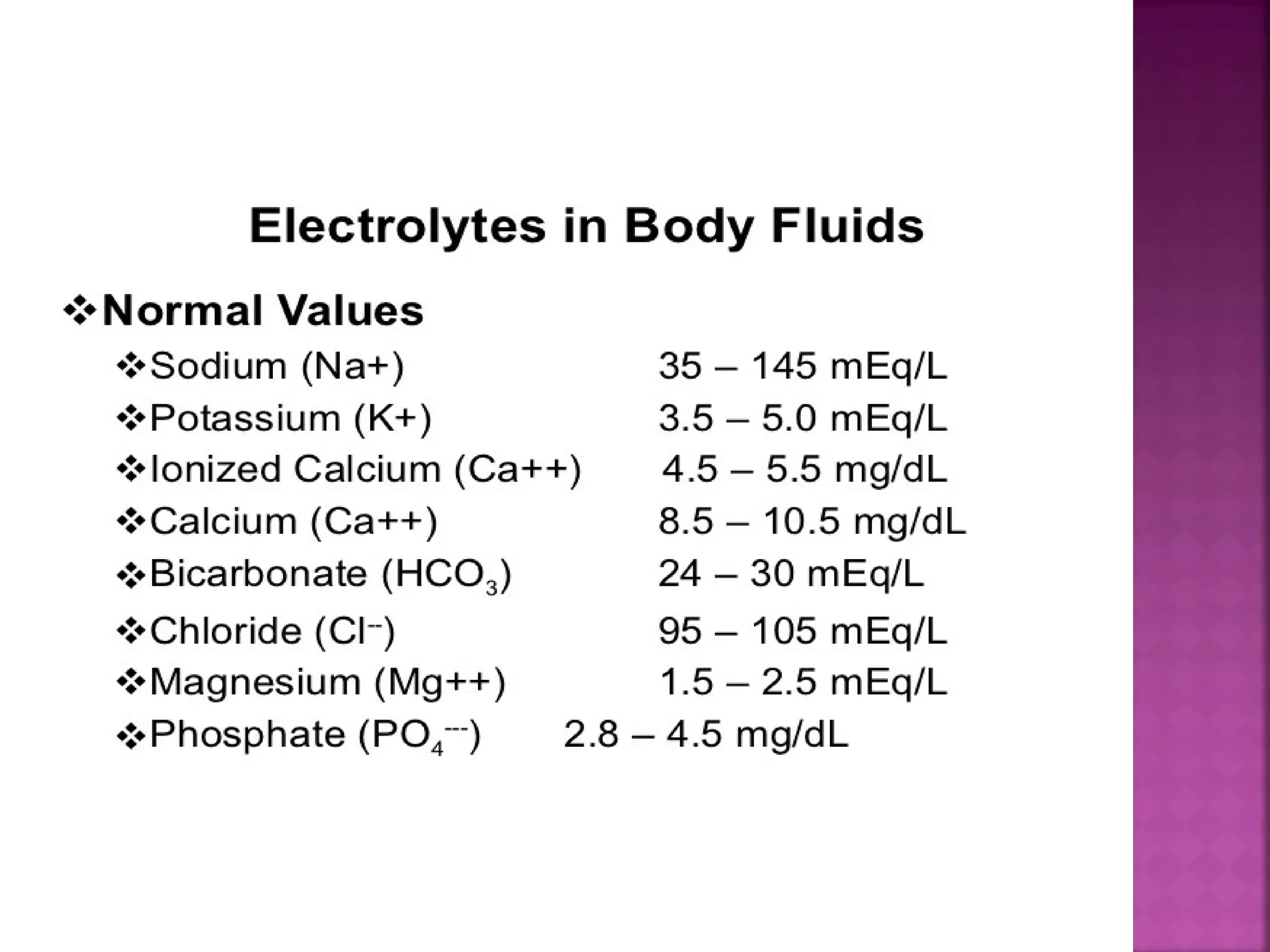
Fluid and electrolyte imbalances can occur when fluid intake and output are not equal. Hypovolemia is a decreased fluid volume, while hypervolemia is an increased fluid volume. Symptoms of hypovolemia include thirst, low blood pressure, and decreased skin turgor. Treatment involves oral or IV fluid replacement depending on severity. Hypernatremia is a high serum sodium level over 145 mEq/L usually due to too much sodium or too little water. It can cause neurological symptoms and death. Treatment focuses on lowering the sodium level through infusion of hypotonic fluids and use of diuretics.