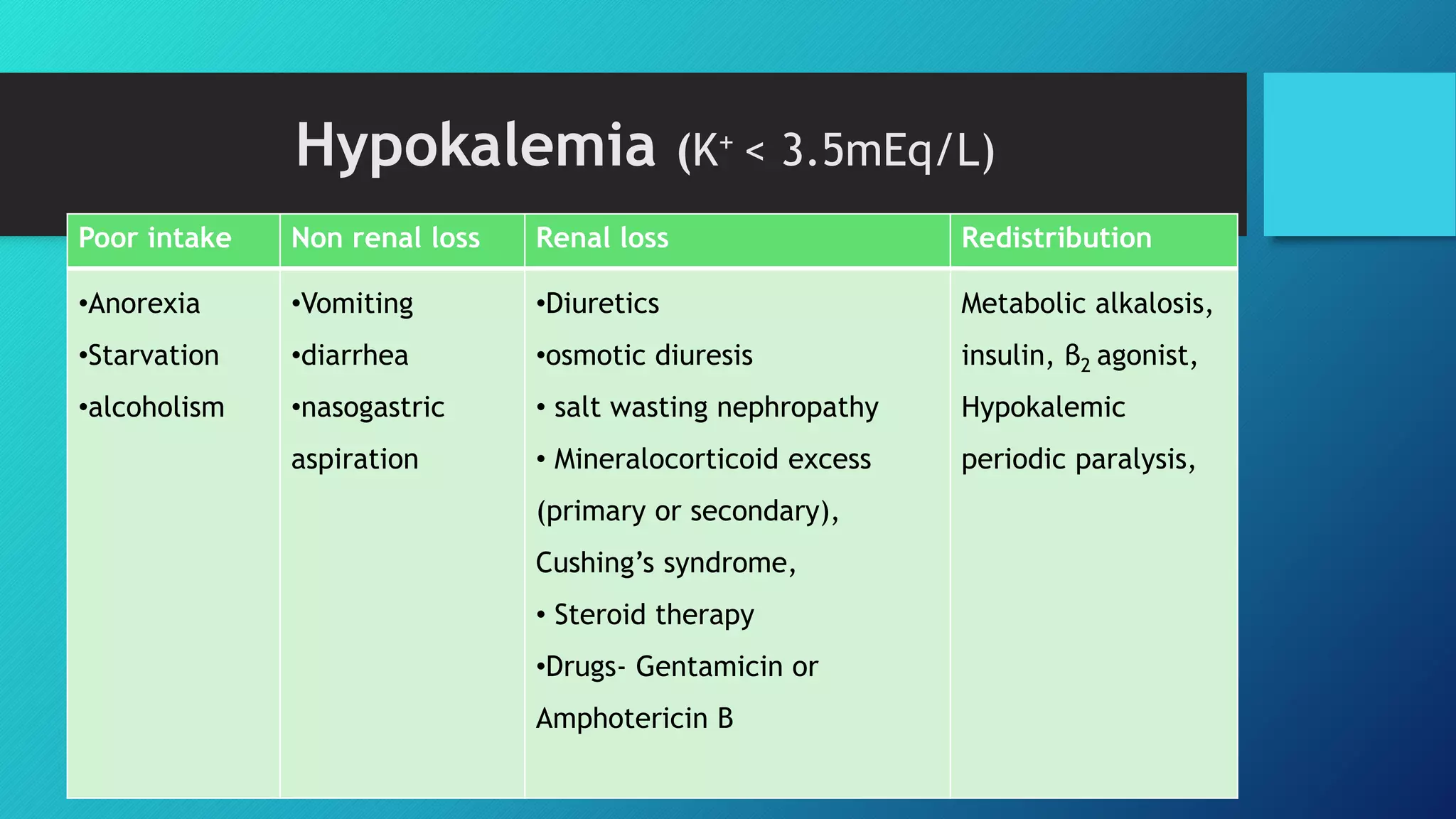
Electrolytes such as sodium, potassium, calcium, and magnesium are important solutes in the body that regulate fluid balance and cell function. Sodium regulates fluid balance and is critical for nerve and muscle function. Hypokalemia can cause muscle weakness while hyperkalemia can cause cardiac arrhythmias. Calcium is needed for muscle and nerve function and its levels are tightly regulated. Magnesium plays a role in many biochemical reactions and body processes. Electrolyte imbalances can cause various clinical manifestations, so it is important to monitor, prevent, and treat electrolyte disorders.



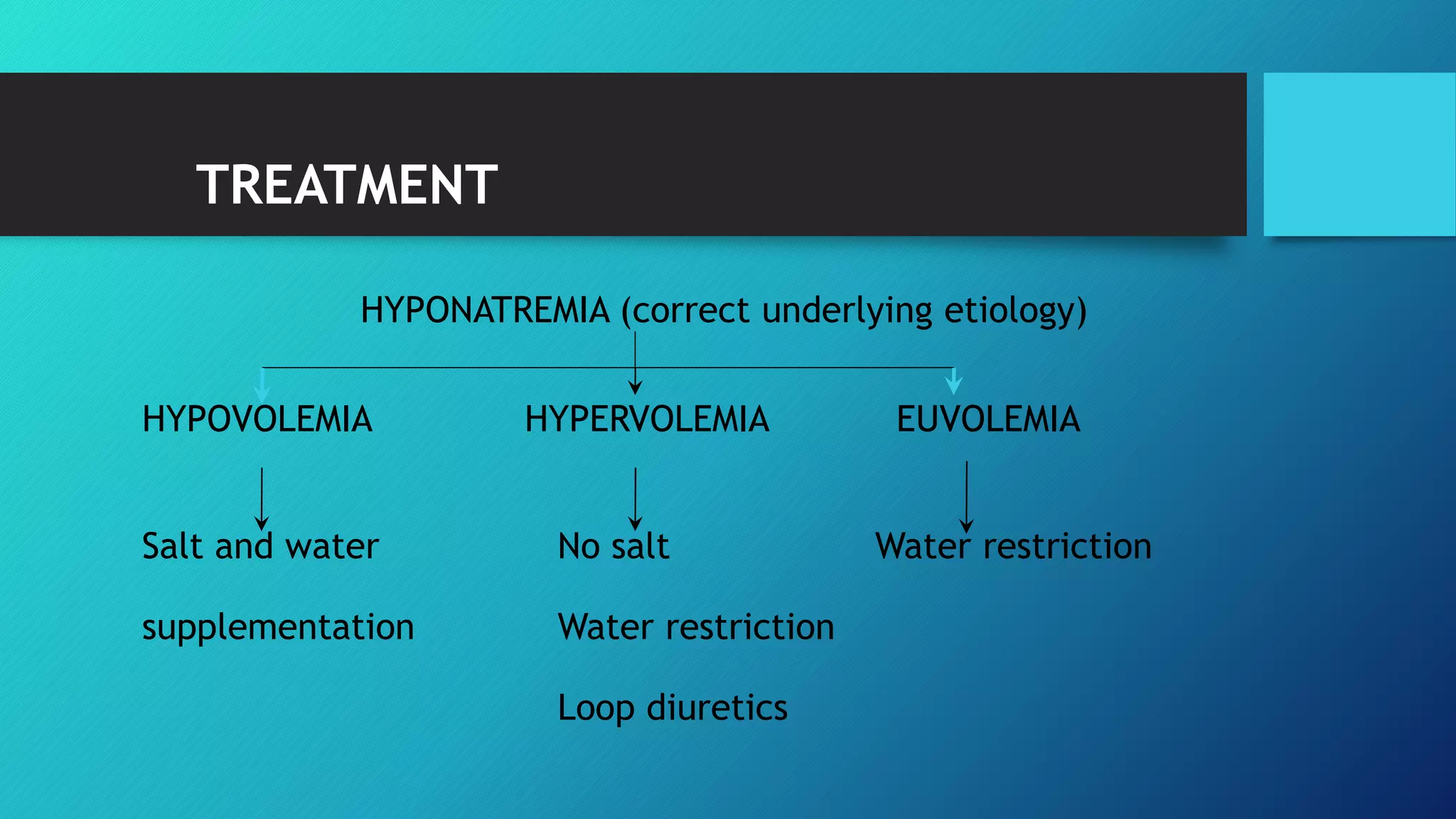




















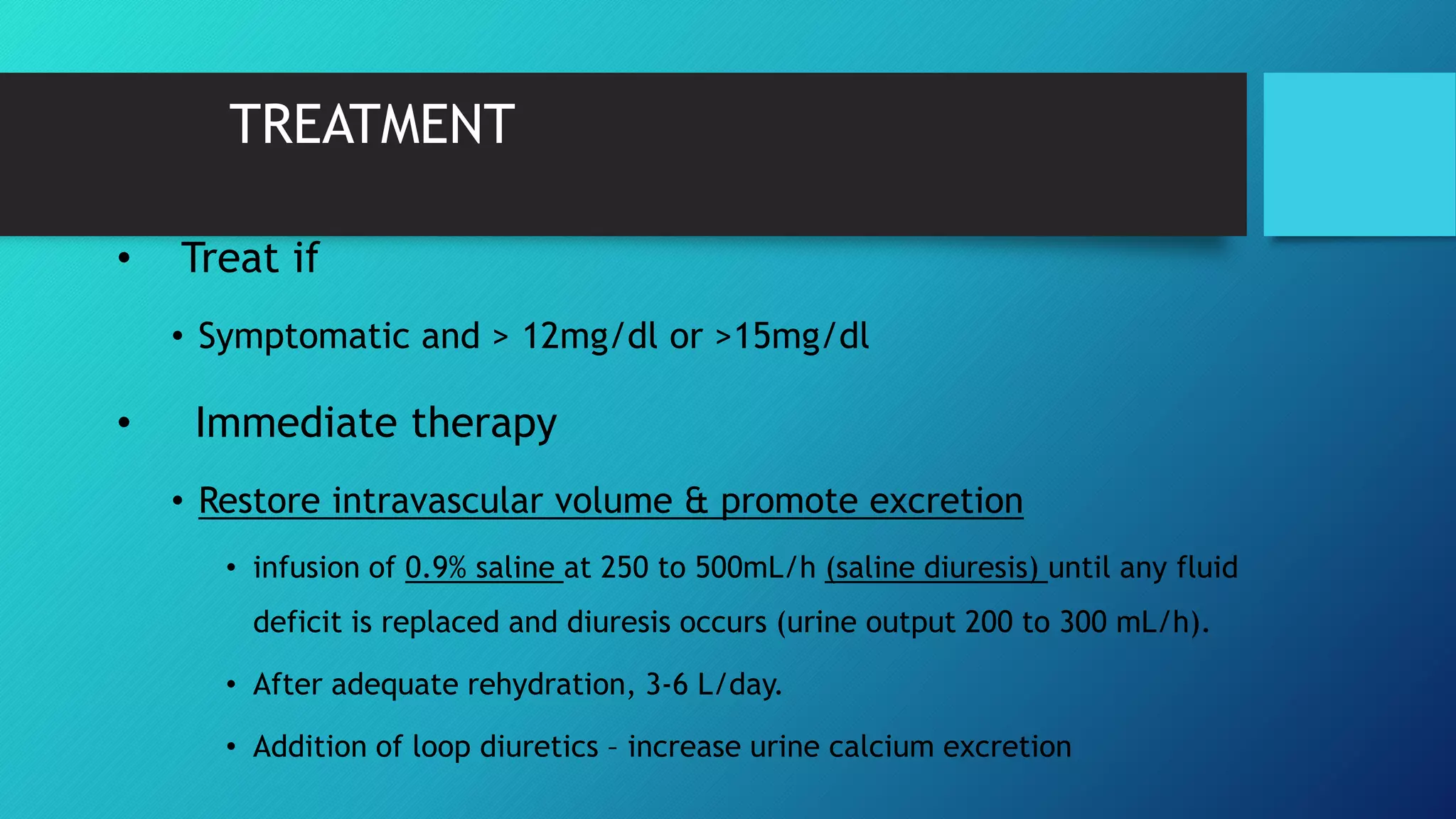







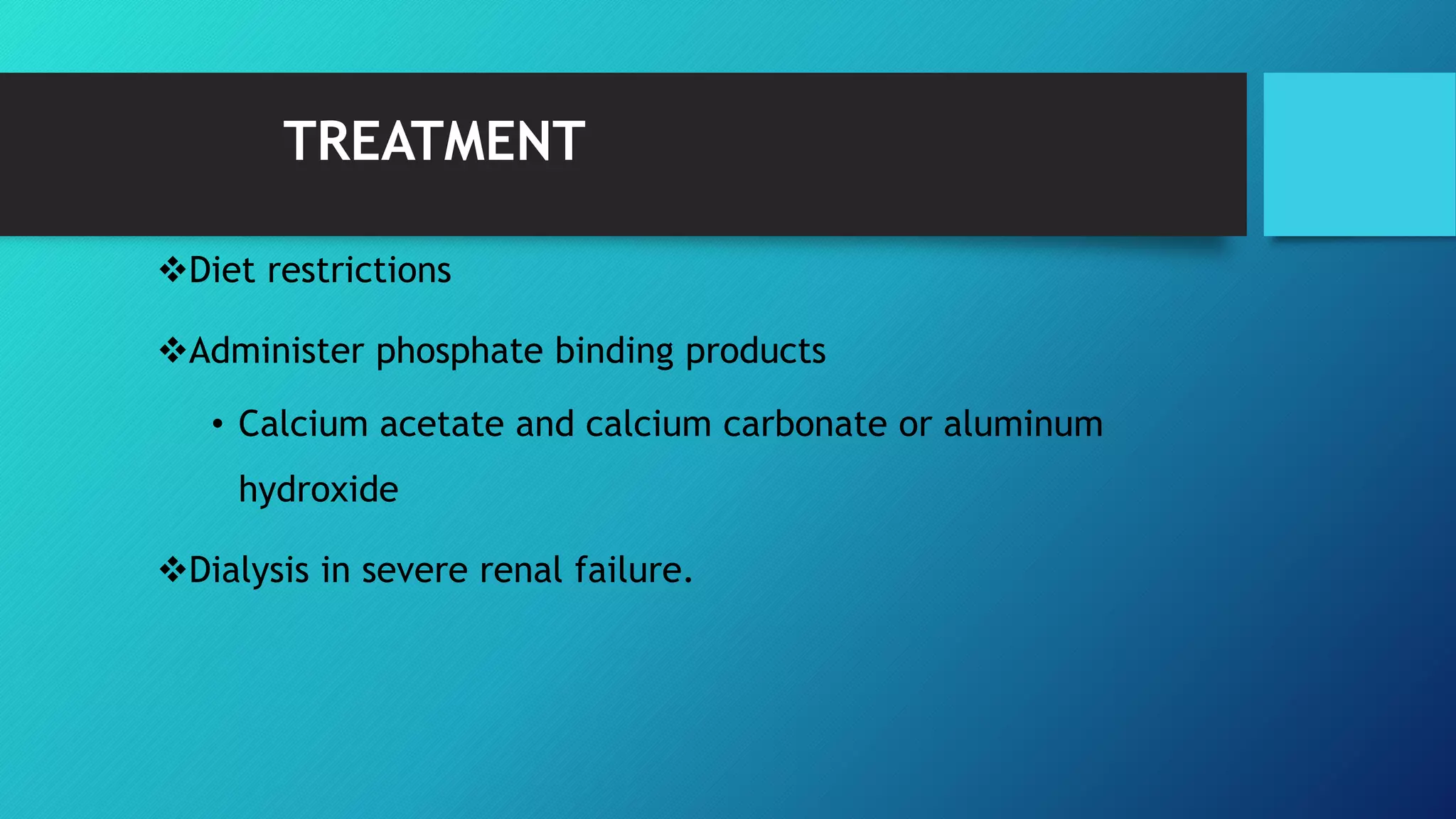
![TREATMENT
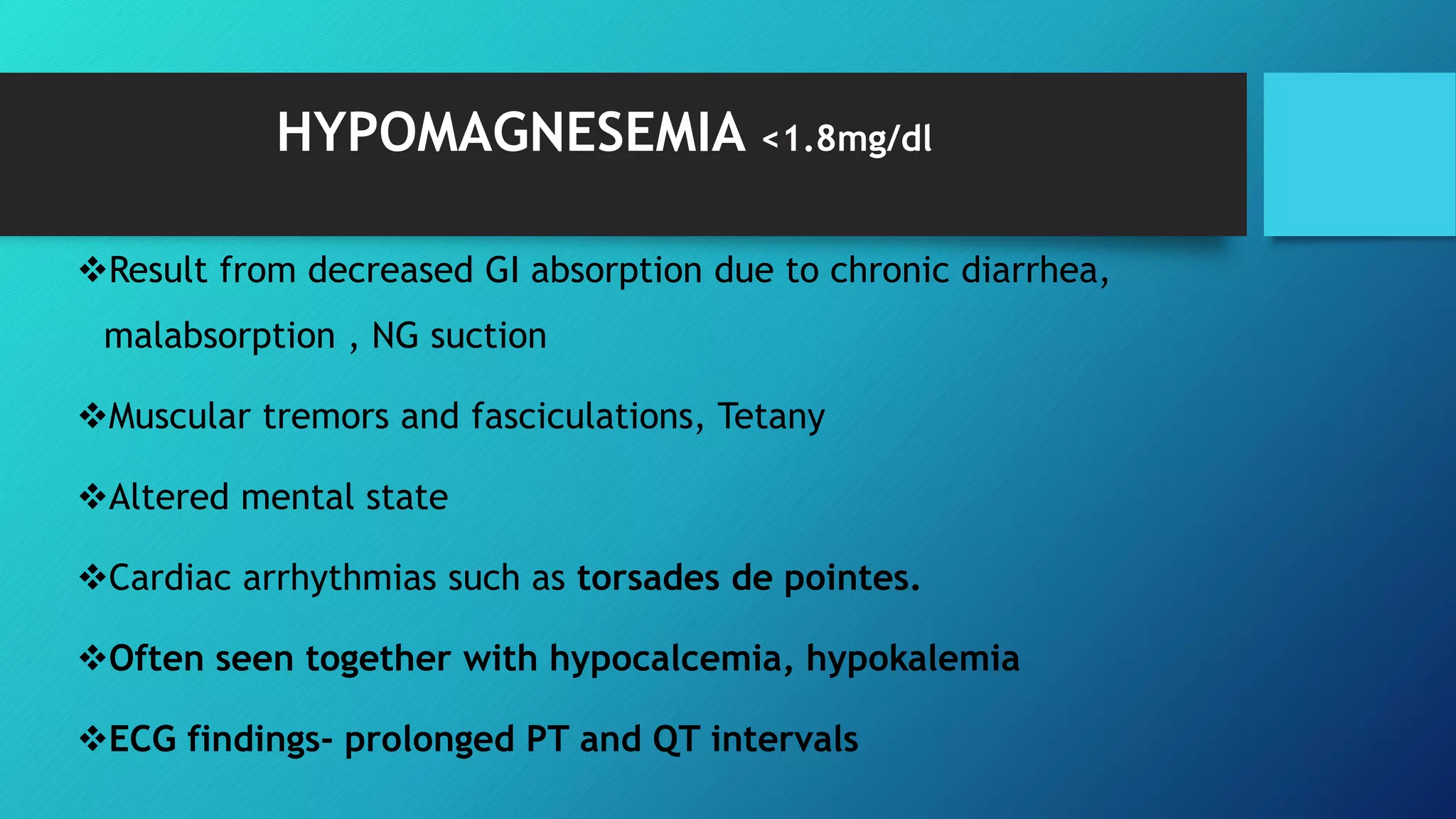
Eliminate source
10% calcium gluconate 10-20 ml IV over 10 min
IV saline diuresis (administration of IV normal saline and furosemide
[1 mg/kg]) can be used to increase renal excretion of magnesium until
dialysis can be performed.
Dialysis is the treatment of choice for severe hypermagnesemia.
Artificial respiration](https://image.slidesharecdn.com/electrolyte-170316173548/75/Electrolyte-and-post-op-fluid-requirement-53-2048.jpg)