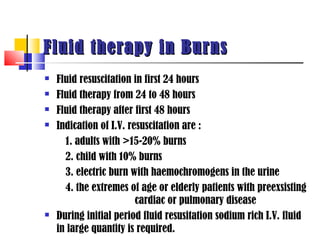
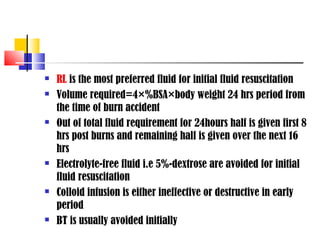
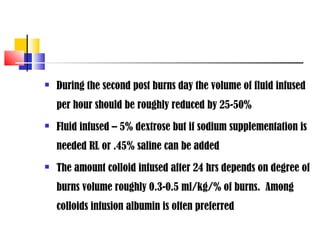
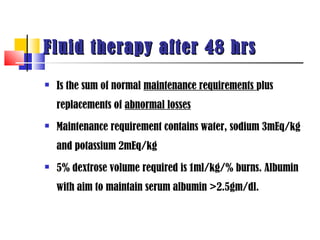
Fluid and electrolyte management is important for perioperative care. Key points include:
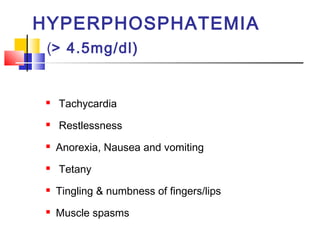
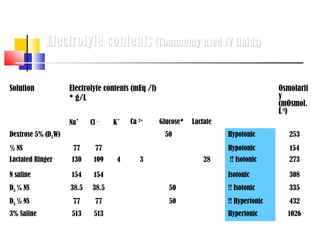
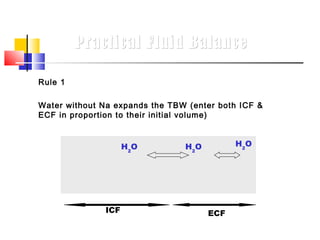
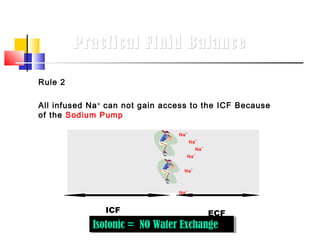
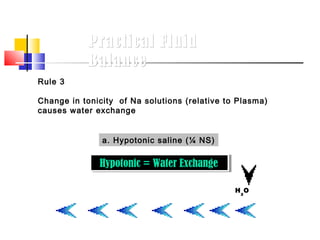
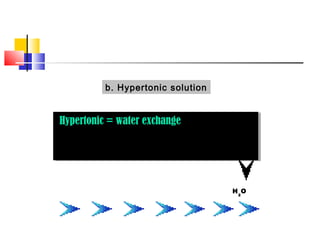
1. Body water is divided into intracellular fluid and extracellular fluid. Common IV fluids contain different electrolyte concentrations and osmolarities.
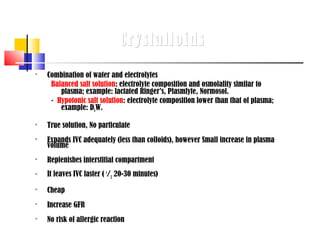
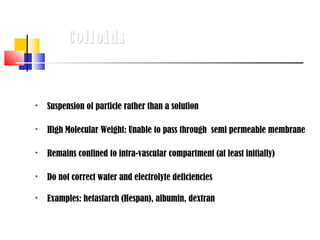
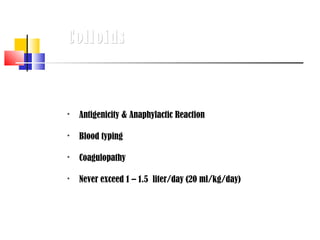
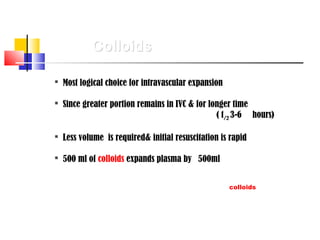
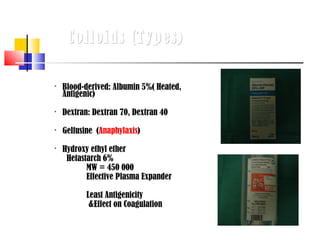
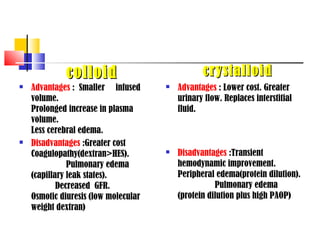
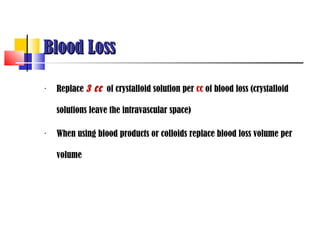
2. Crystalloids expand plasma volume but leave the intravascular space quickly, while colloids remain intravascular longer but do not correct electrolyte deficiencies.
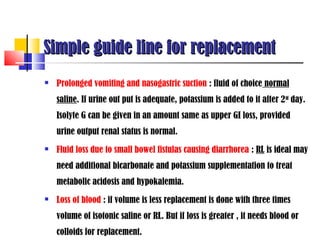
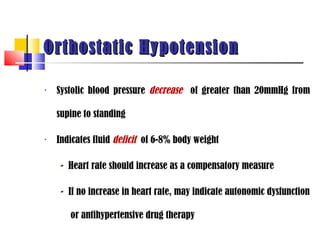
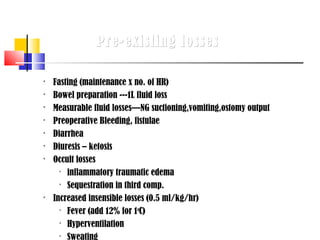
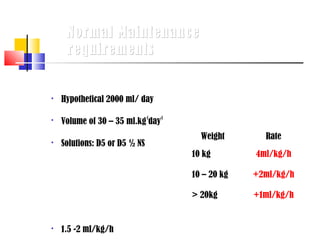
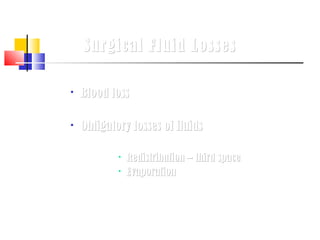
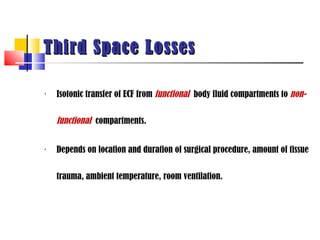
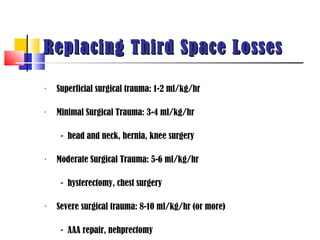
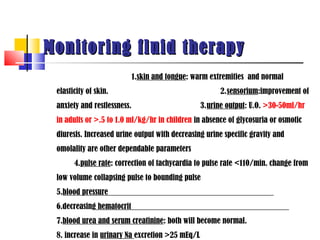
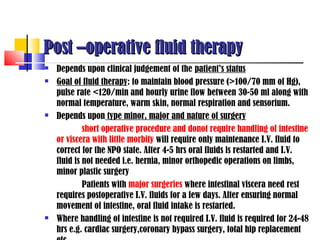
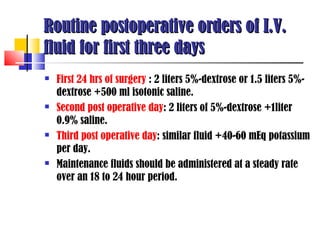
3. Perioperative fluid management aims to replace pre-existing deficits, normal maintenance needs, and abnormal surgical losses like blood loss, third spacing, and insensible losses. Close monitoring of fluid status is important.
![Body Water Compartments
• Intracellular water: 2/3 (40%)of TBW
• Extracellular water: 1/3 (20%)of TBW
- Extravascular water[interstitial]: 3/4 (15%)of extracellular
water
- Intravascular water[plasma]: 1/4 (5%)of extracellular
water](https://image.slidesharecdn.com/fluidandelectrolytemanagement-130207031856-phpapp02/85/Fluid-and-electrolyte-management-2-320.jpg)

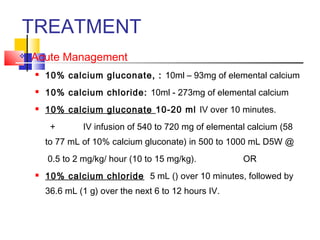
![…TREATMENT
Severe elevation (7 mEq/L with toxic ECG
changes)
Calcium chloride (10%) 500 to 1000 mg (5 to 10 mL) IV
over 2 to 5 minutes or Calcium Gluconate 10% 10-20ml
over 5-10mins
to reduce the effects of potassium at the myocardial cell
membrane (lowers risk of ventricular fibrillation [VF])
Avoid if patient is on digitalis.](https://image.slidesharecdn.com/fluidandelectrolytemanagement-130207031856-phpapp02/85/Fluid-and-electrolyte-management-68-320.jpg)

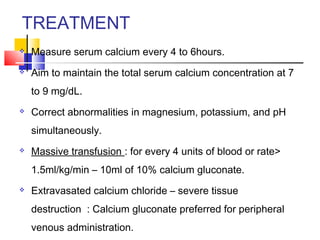
![TREATMENT
Eliminate source
10% calcium chloride (5 to 10 mL [500 to 1000 mg] IV) or 10%
calcium gluconate will often correct lethal arrhythmias.
IV saline diuresis (administration of IV normal saline and furosemide
[1 mg/kg]) can be used to increase renal excretion of magnesium
until dialysis can be performed.
Dialysis is the treatment of choice for severe hypermagnesemia.
Artificial respiration](https://image.slidesharecdn.com/fluidandelectrolytemanagement-130207031856-phpapp02/85/Fluid-and-electrolyte-management-92-320.jpg)