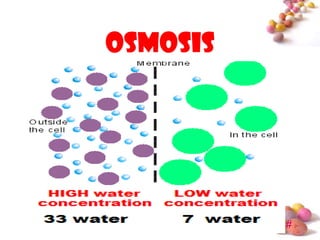
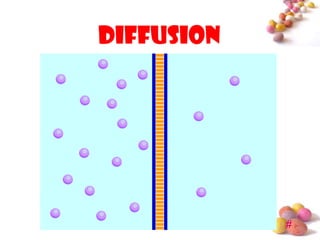
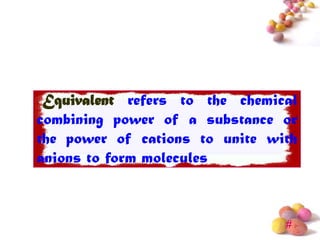
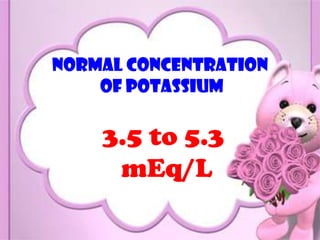
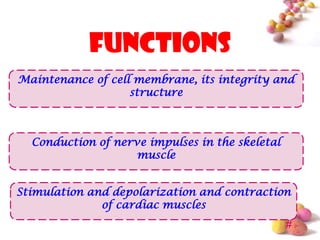
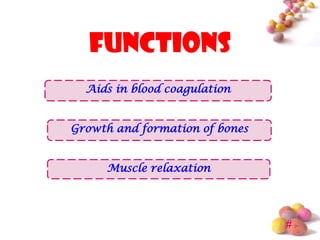
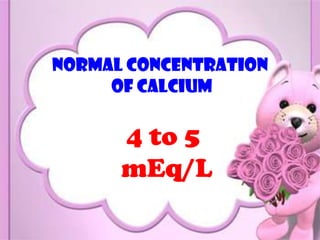
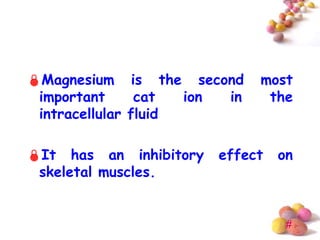
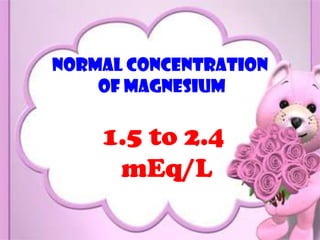
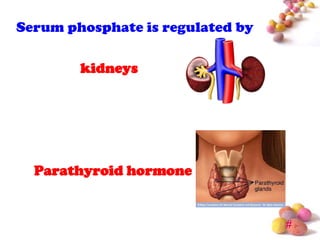
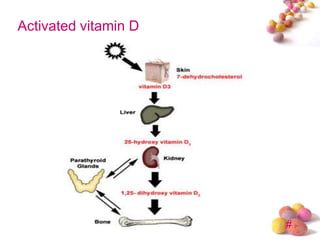
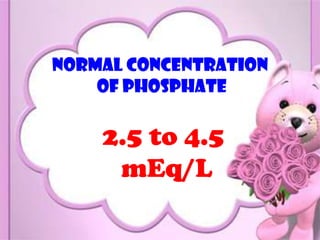
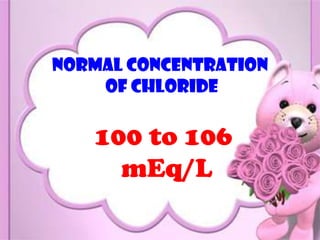
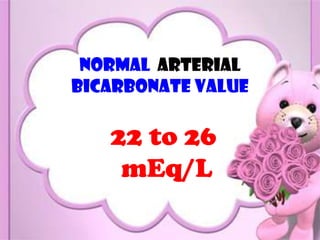
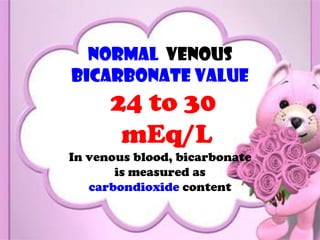
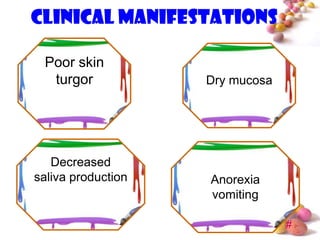
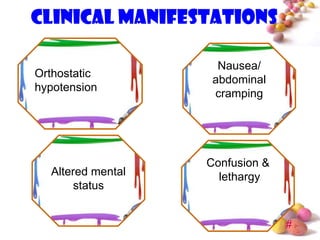
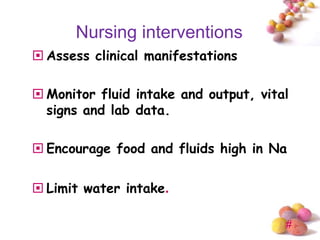
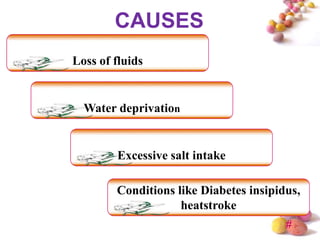
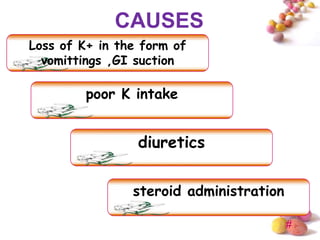
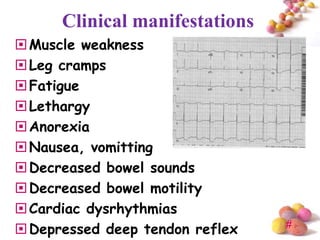
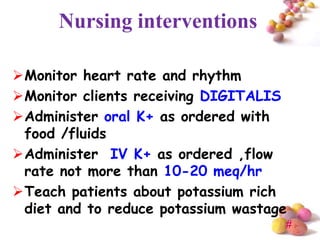
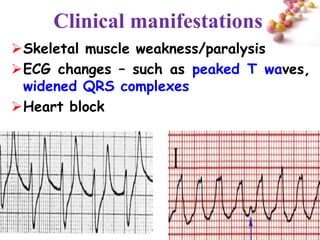
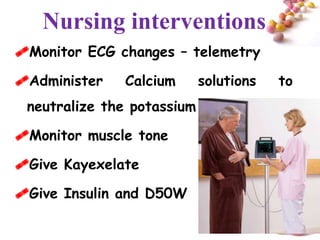
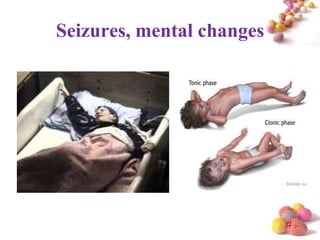
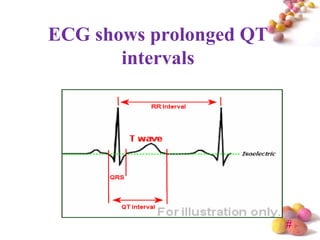
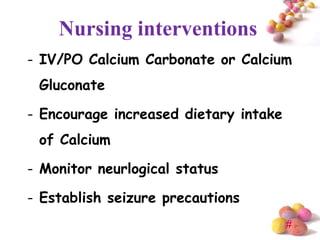
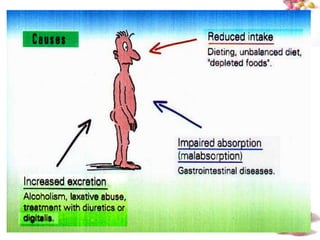
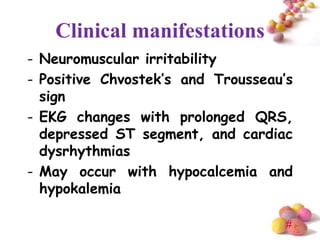
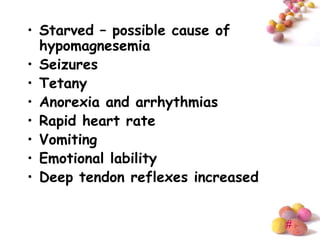
This document discusses fluid and electrolyte balance and disturbances. It covers the mechanisms of fluid and electrolyte movement including osmosis, diffusion, and filtration. It then discusses sodium, potassium, calcium, magnesium, chloride, bicarbonate, and phosphate levels and imbalances including causes, clinical manifestations, and nursing interventions for conditions like hyponatremia, hypernatremia, hypokalemia, hyperkalcemia, hypocalcemia, hypercalcemia, hypomagnesemia, and hypermagnesemia. Food sources of important electrolytes are also provided.