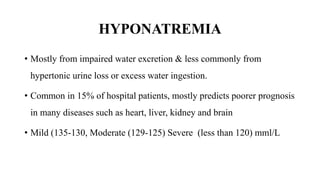
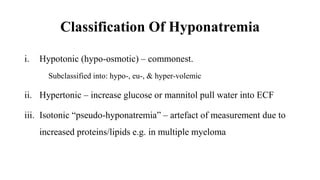
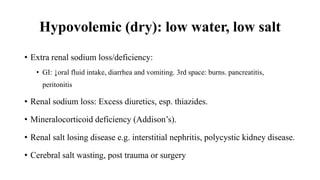
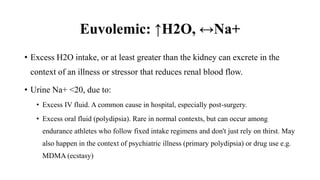
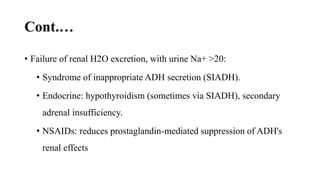
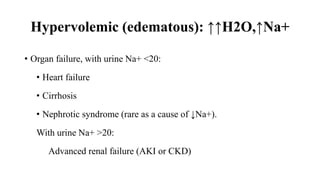
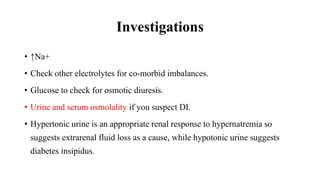
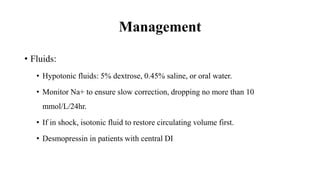
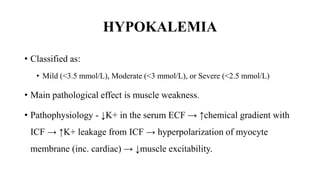
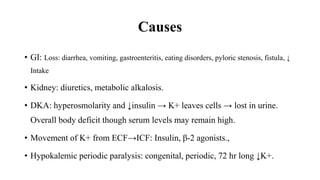
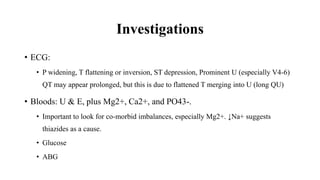
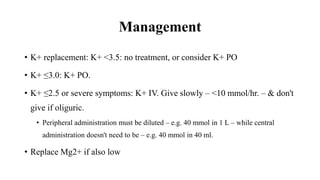
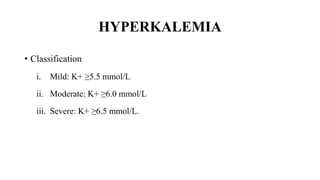
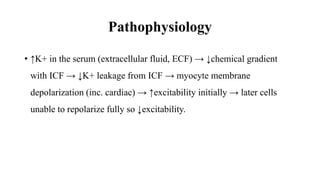
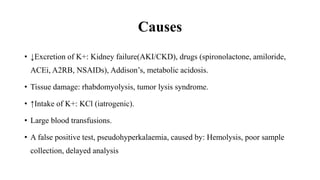
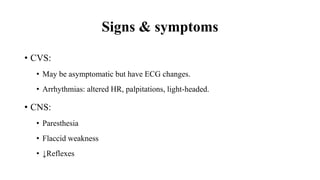
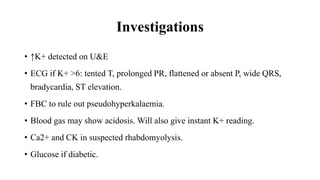
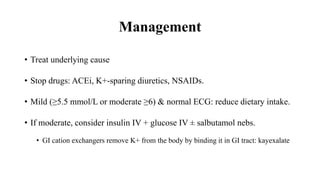
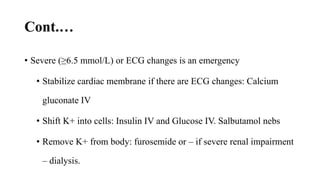
This document discusses electrolyte imbalances focusing on sodium and potassium. It covers the causes, signs, symptoms, investigations, and management of hyponatremia, hypernatremia, hypokalemia, and hyperkalemia. Specifically, it classifies the severity of the imbalances and describes the pathophysiology involving fluid shifts between extracellular and intracellular compartments. It provides detailed guidelines for evaluating patients and correcting electrolyte abnormalities through fluid management and medication.