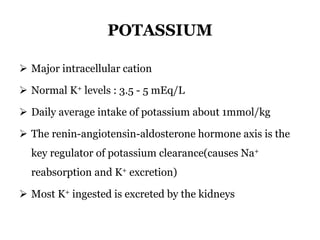
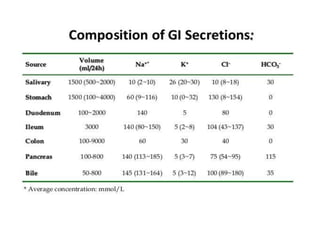
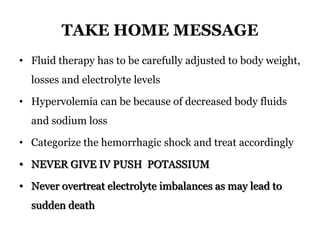
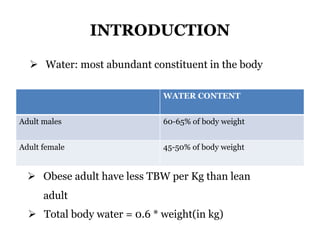
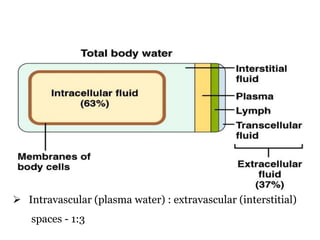
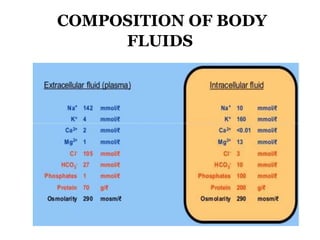
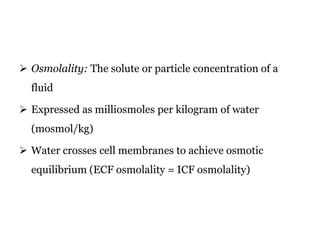
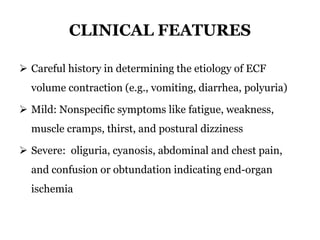
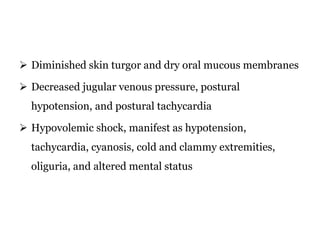
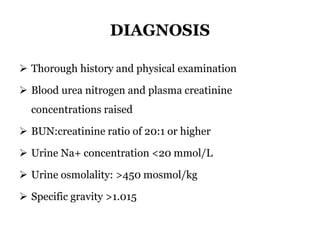
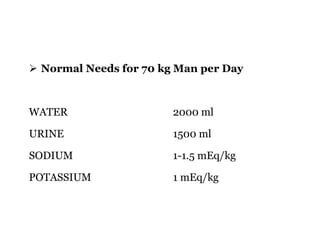
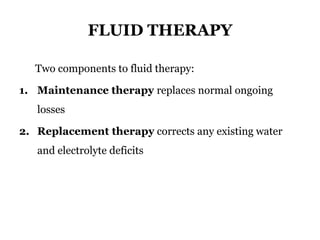
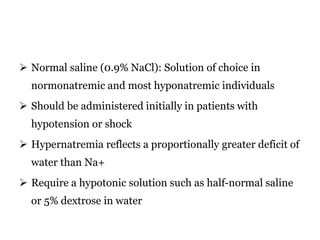
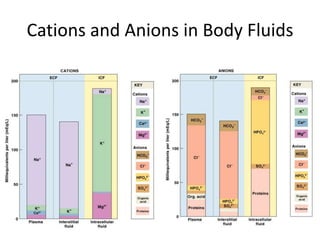
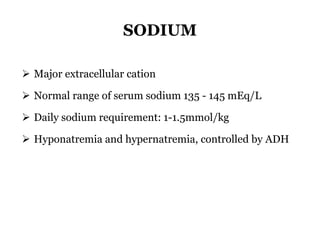
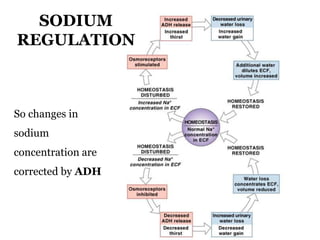
1) Fluid and electrolyte balance is essential for human health and involves complex regulation of water and electrolytes like sodium and potassium in the body.
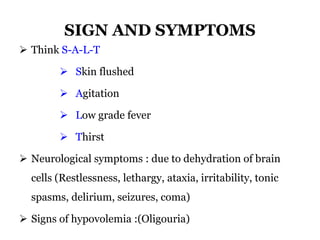
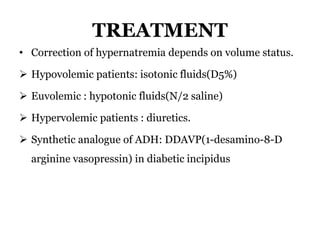
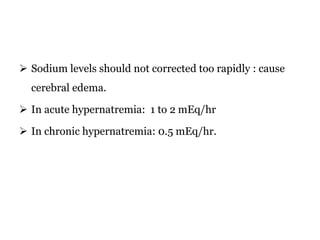
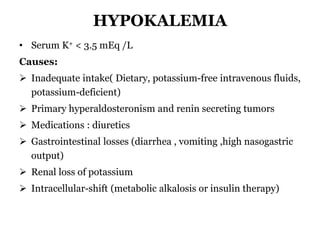
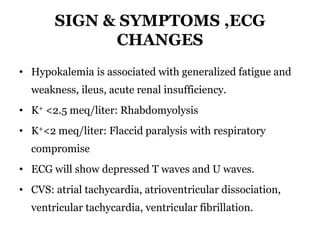
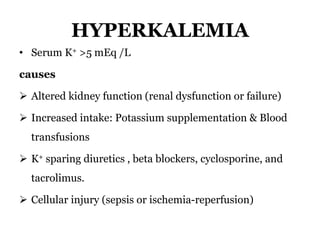
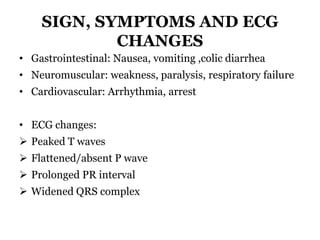
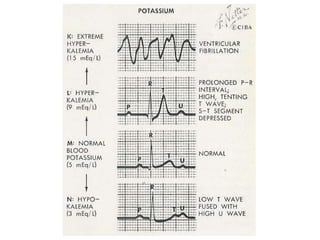
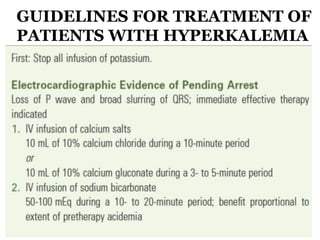
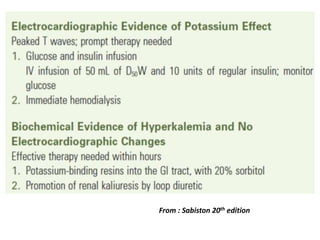
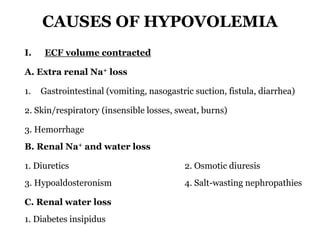
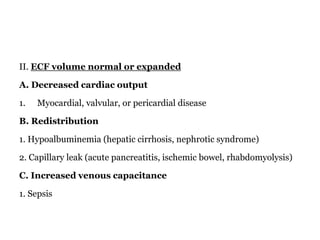
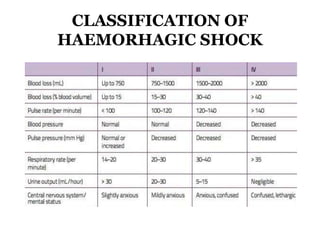
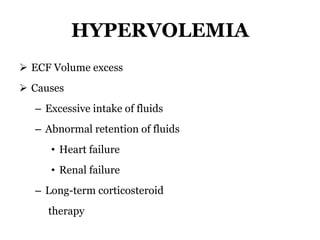
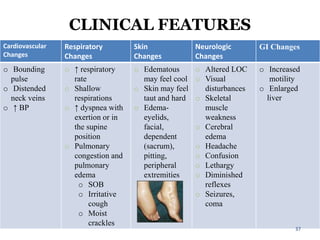
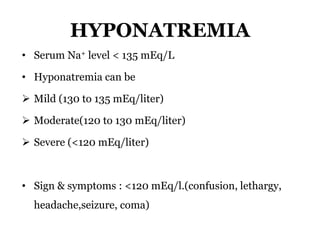
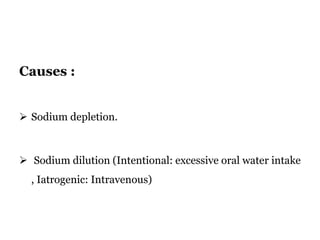
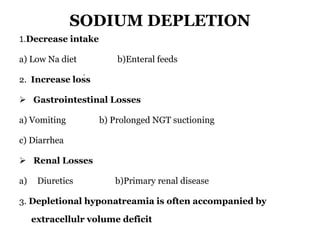
2) Imbalances can cause hypo- or hypervolemia and issues like hyponatremia or hyperkalemia.
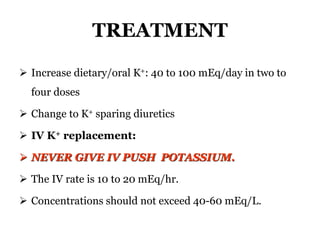
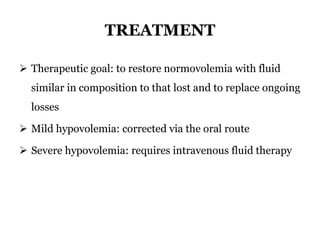
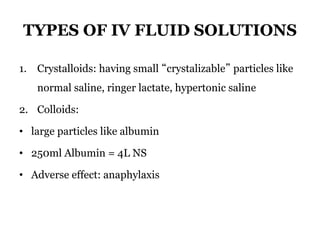
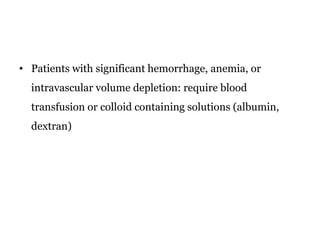
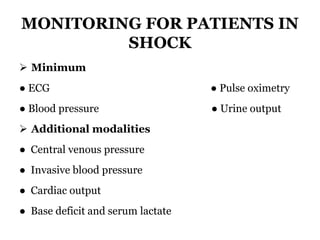
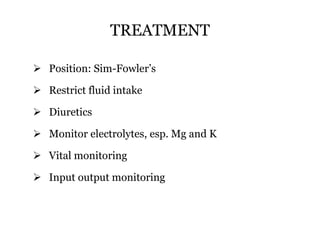
3) Treatment depends on the cause and aims to restore normal fluid volume and electrolyte levels, using oral or IV fluids and monitoring for complications.
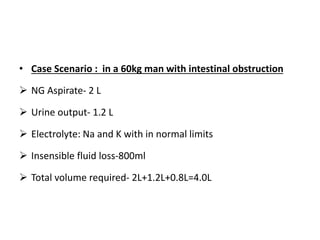
![REPLACEMENT THERAPY
Total water loss in the form of vomiting, loose stools,
inadequate intake of fluid, insensible water loss
Usually given as a bolus of 2 liters
Free water deficit = (([Na]/140) − 1) × TBW](https://image.slidesharecdn.com/fluidandelectrolyte-181114092953/85/Fluid-and-electrolyte-27-320.jpg)

![TREATMENT
Sodium Deficit:
Sodium deficit (mEq) = [Na+] goal − [Na+] plasma x0.6xbodyweight
Ex- 60kg male with s.sodium 125mEq
Sodium deficit (mEq) =(140mEq-125mEq)x.6x60=540mEq
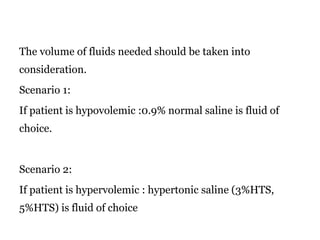
Infusion of normal saline 0.9%, hypertonic (HTS) may be required.
HTS is available commercially(in 3%, 5% concentrations)](https://image.slidesharecdn.com/fluidandelectrolyte-181114092953/85/Fluid-and-electrolyte-47-320.jpg)