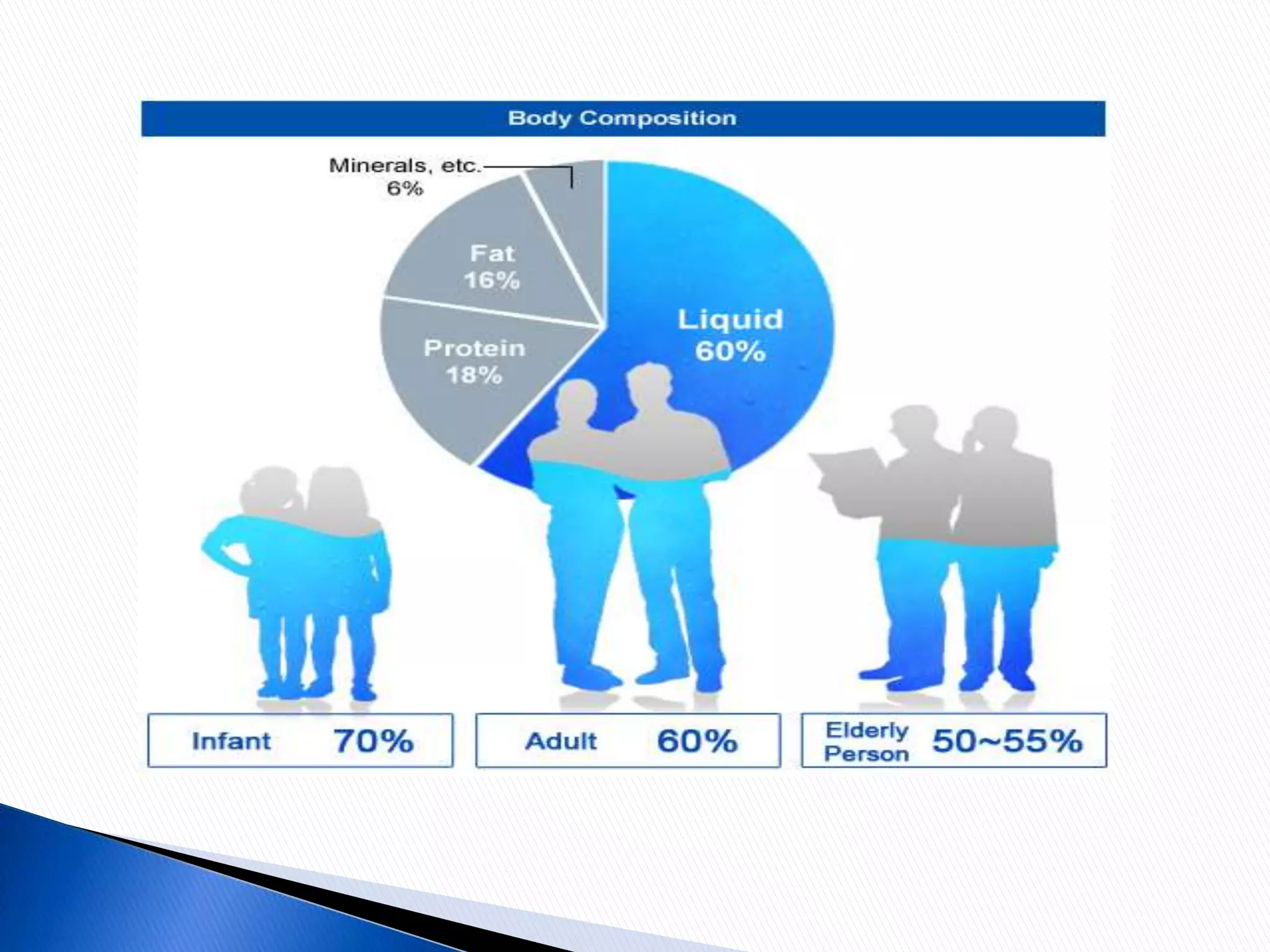
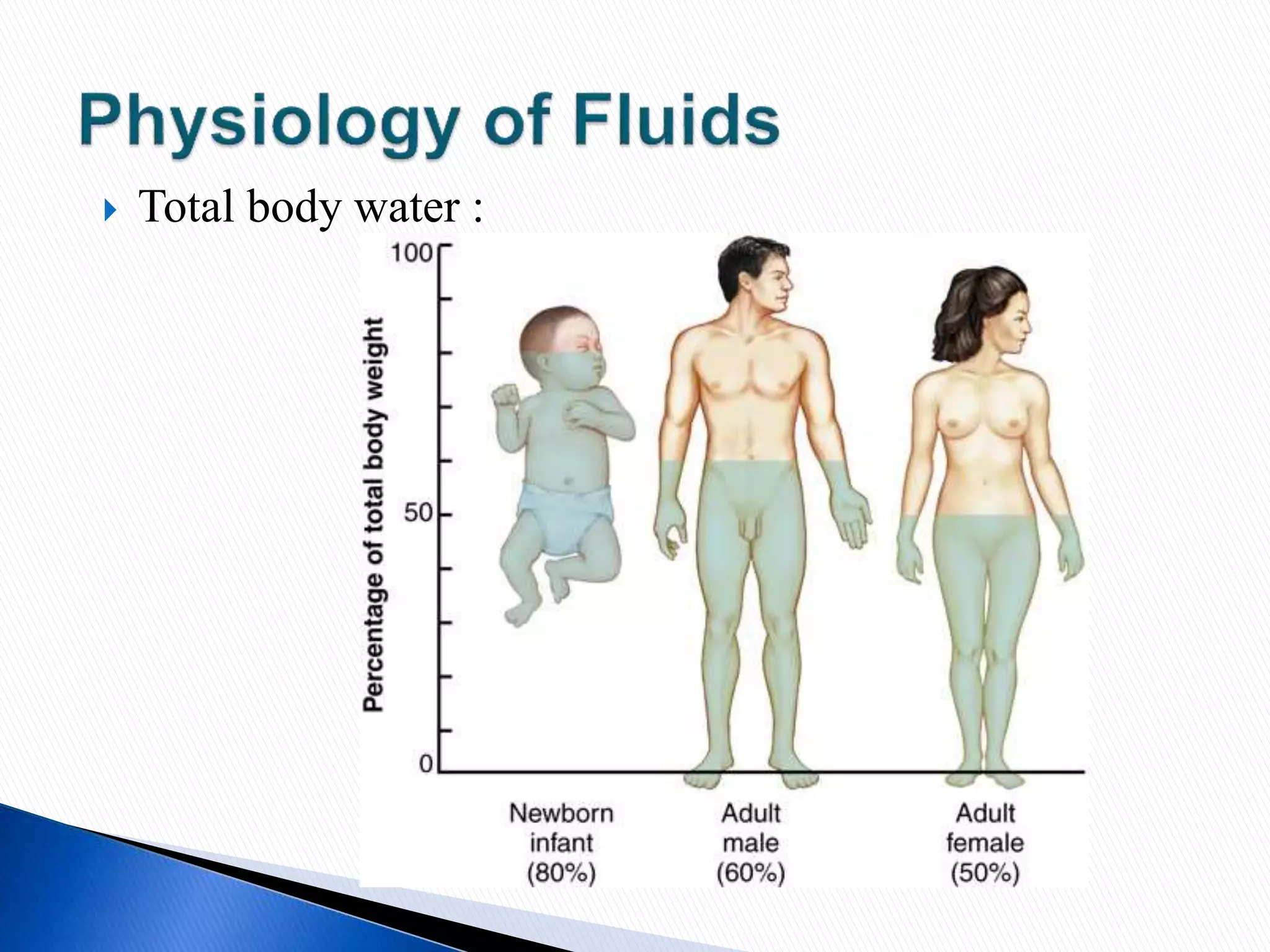
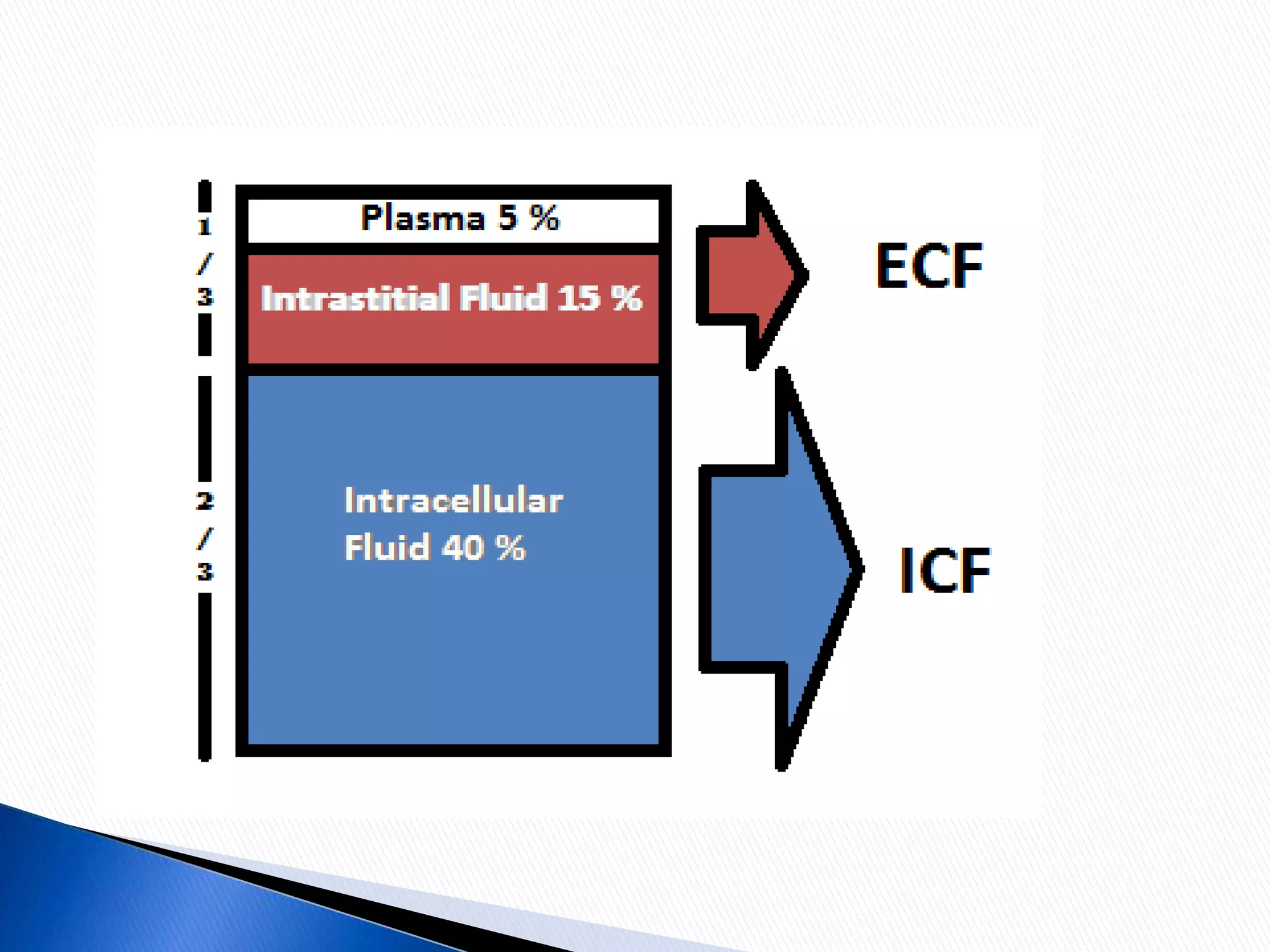
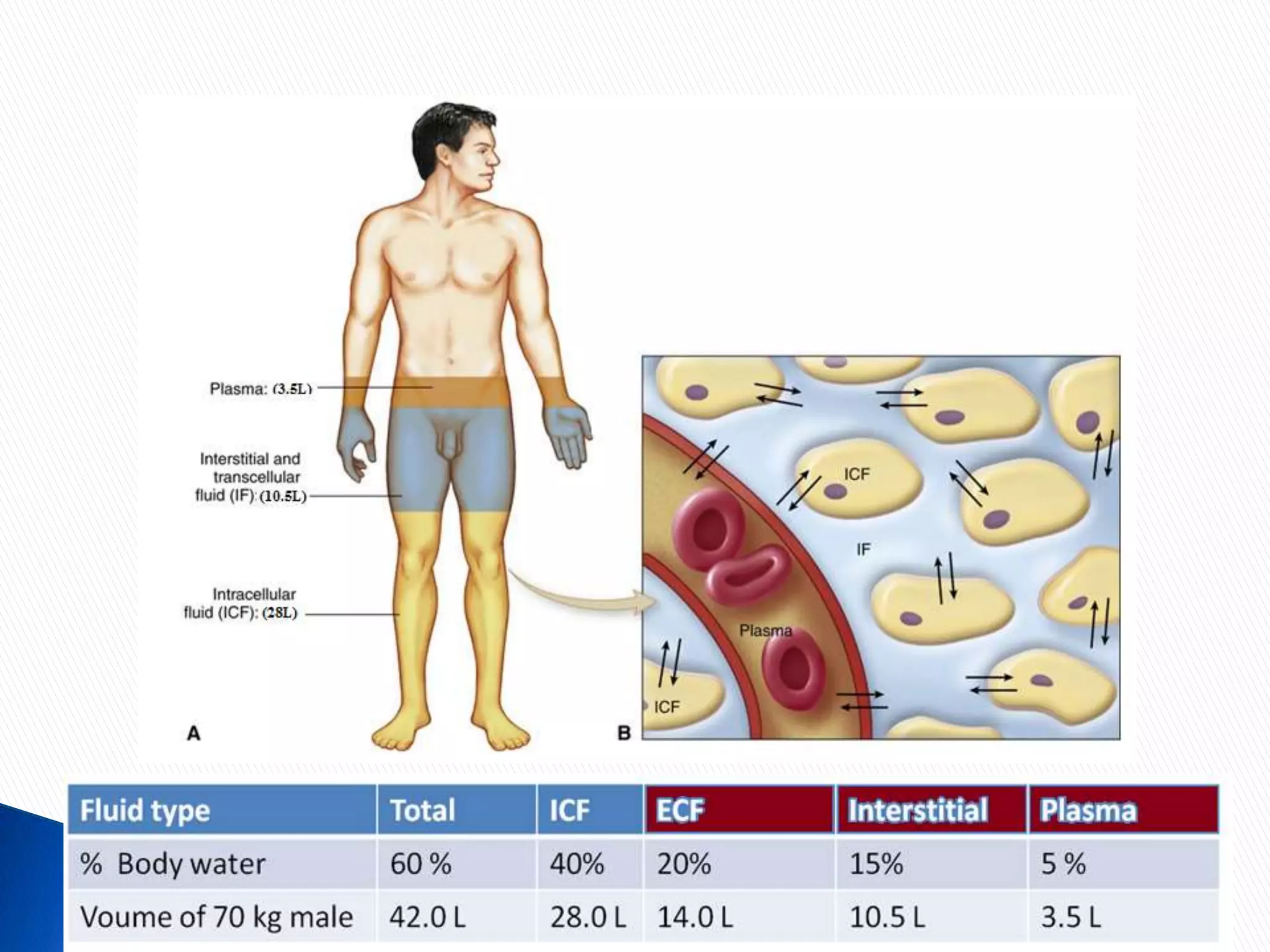
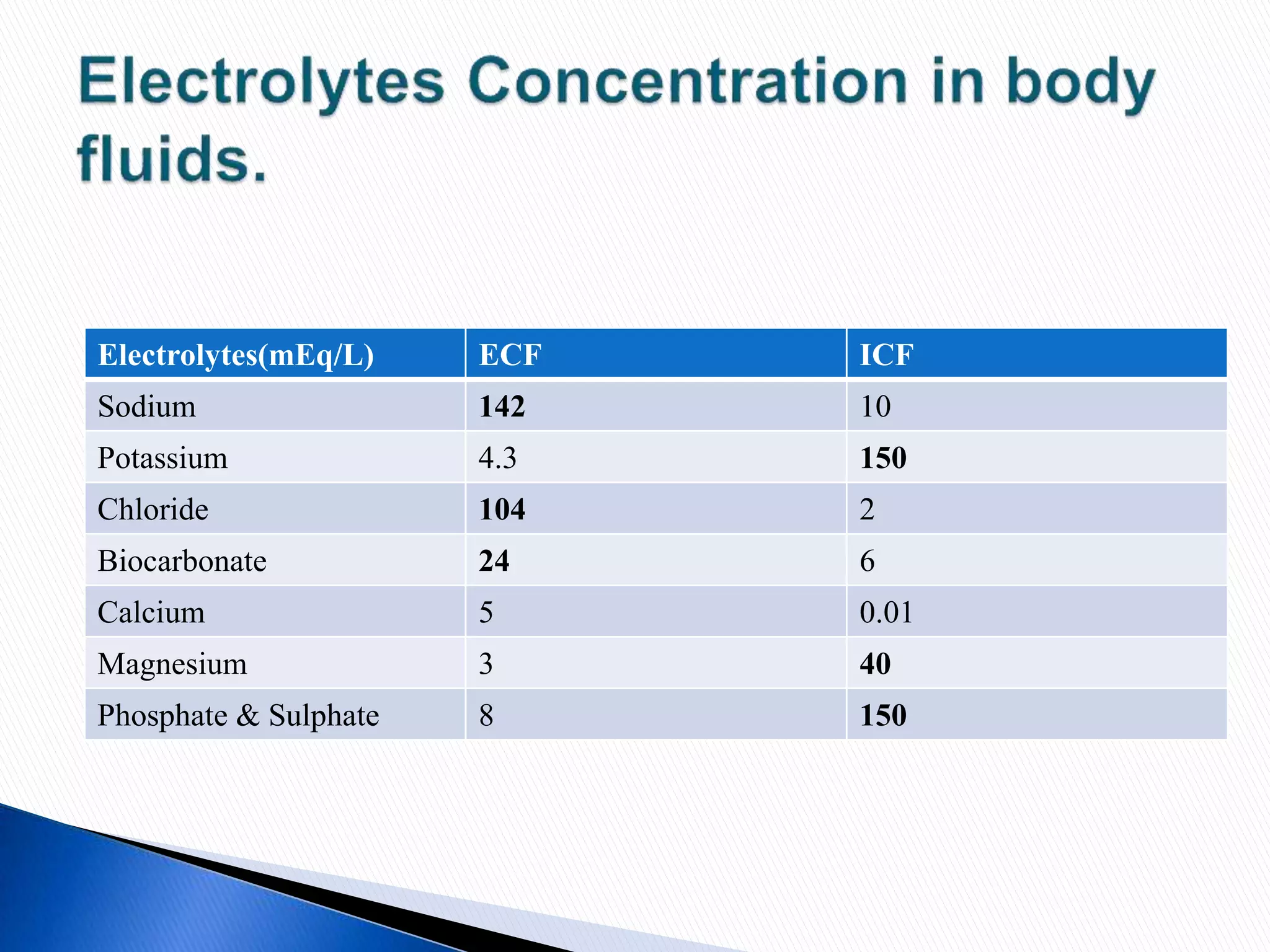
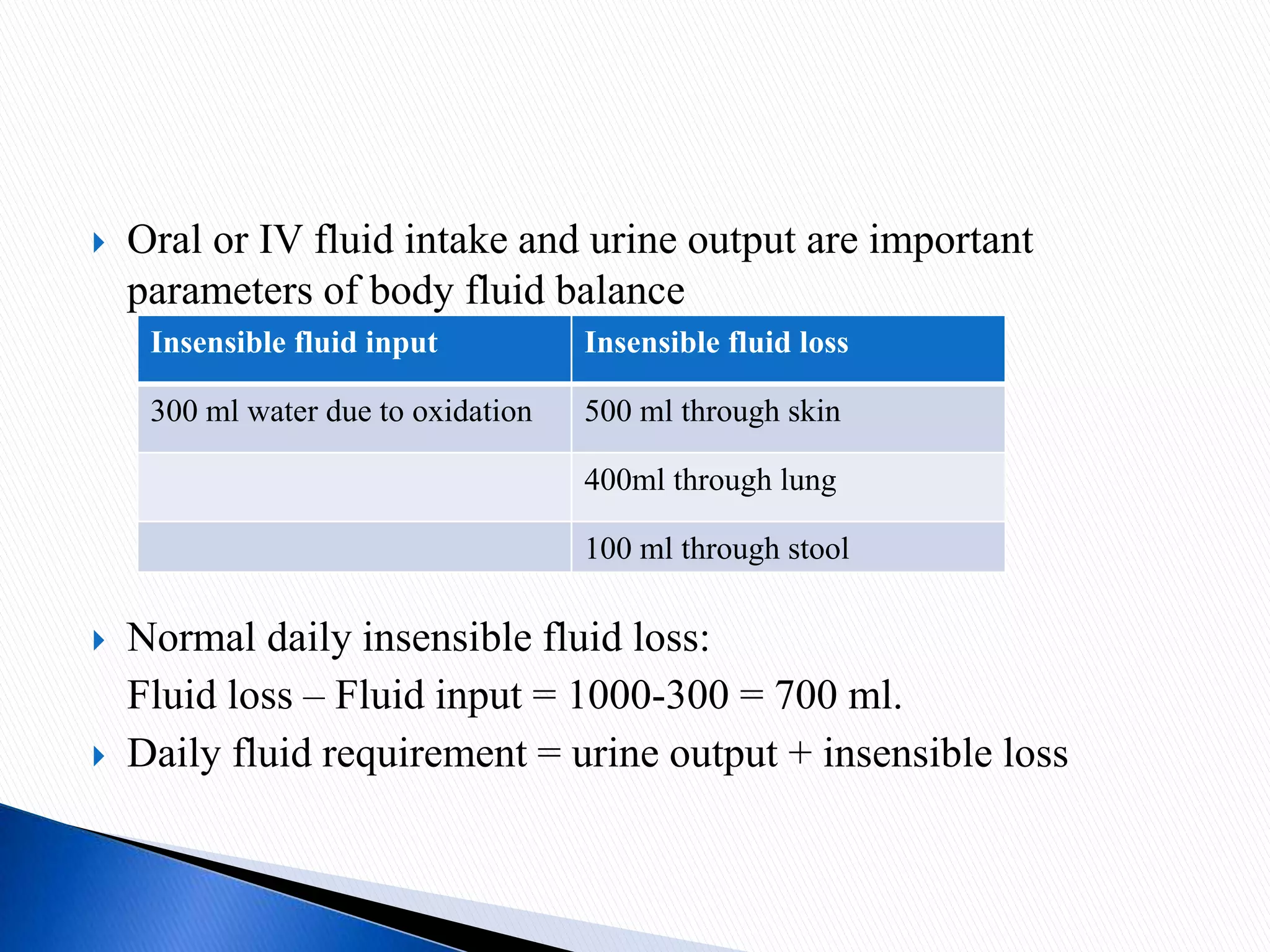
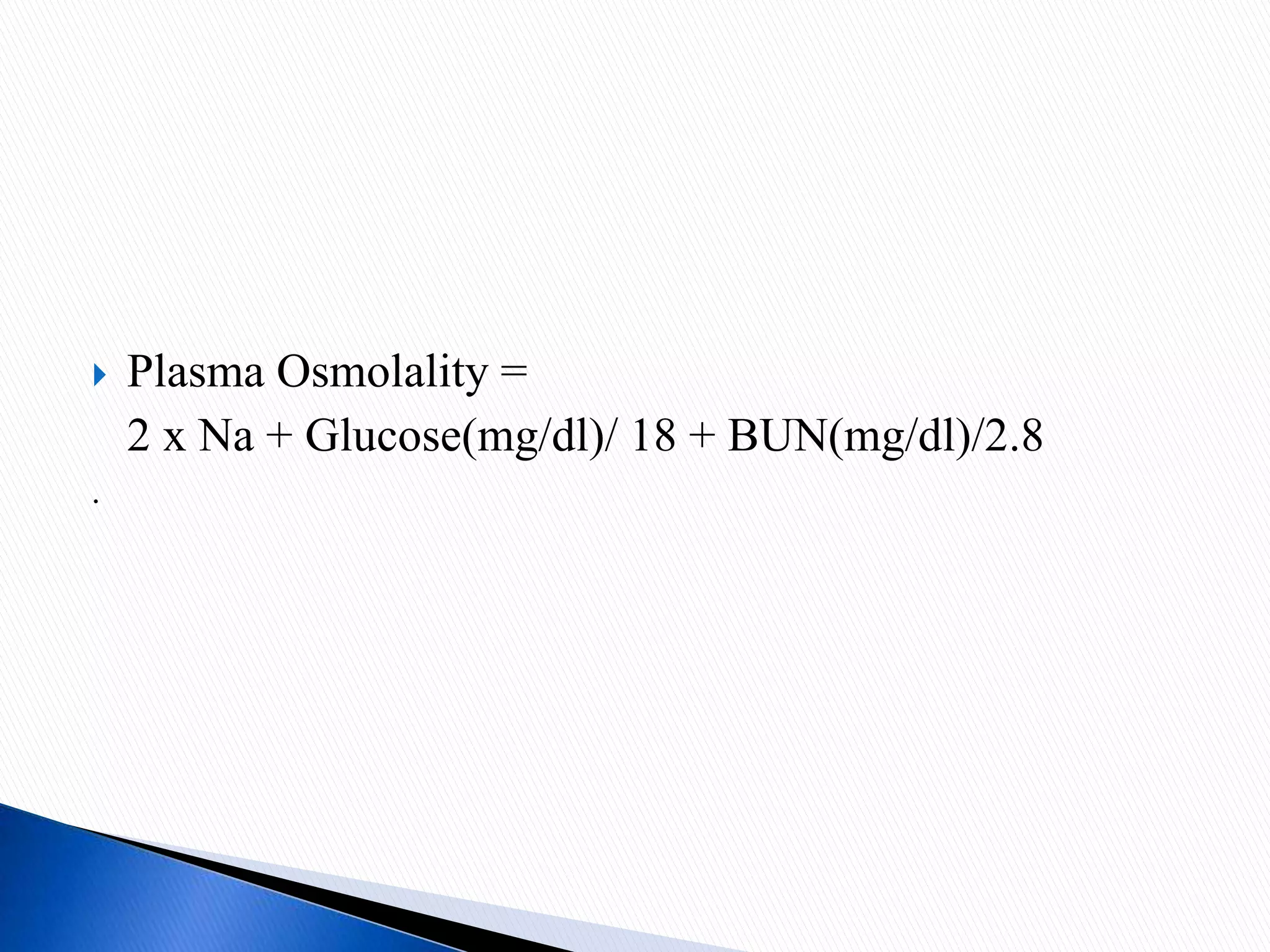
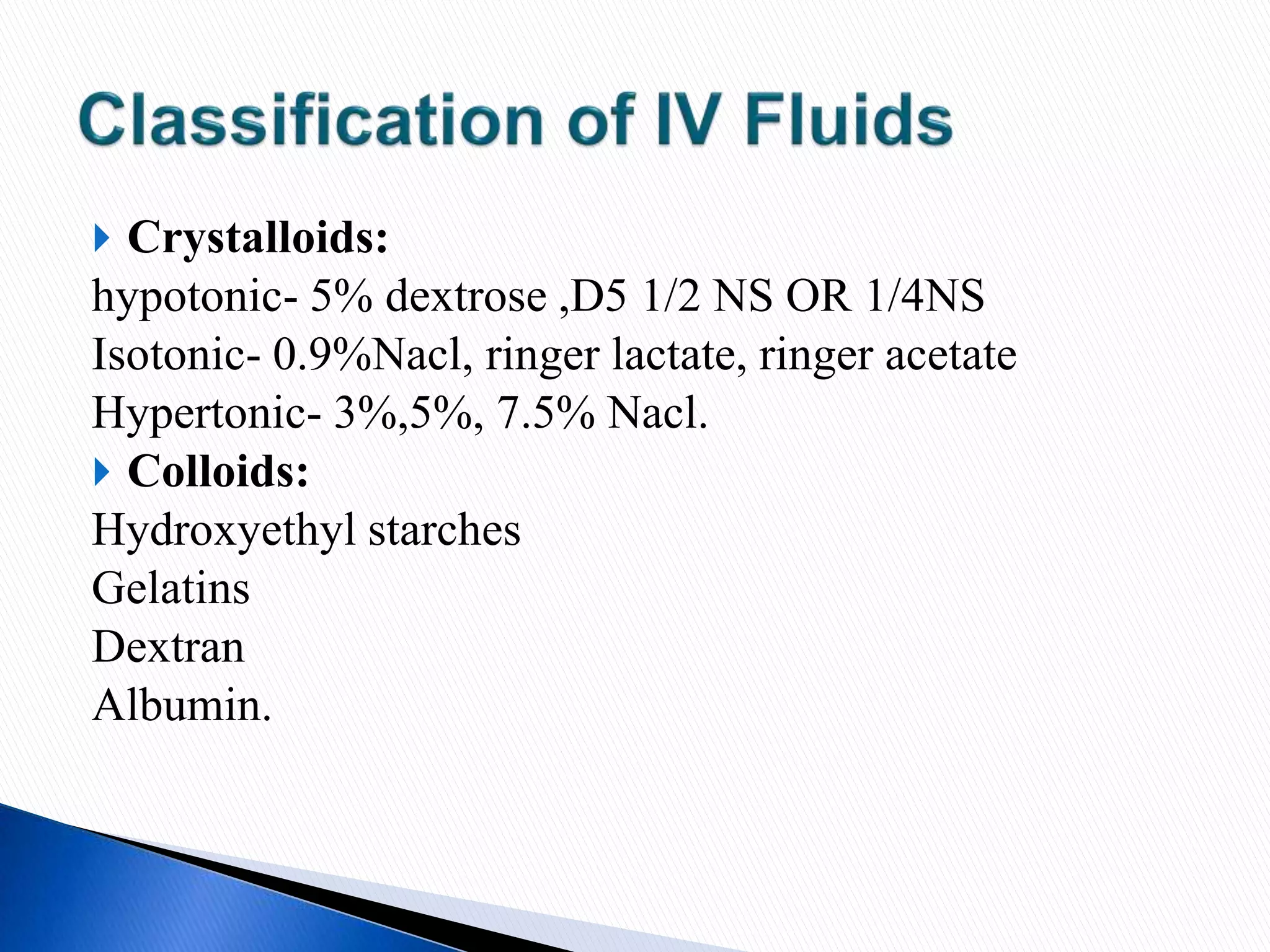
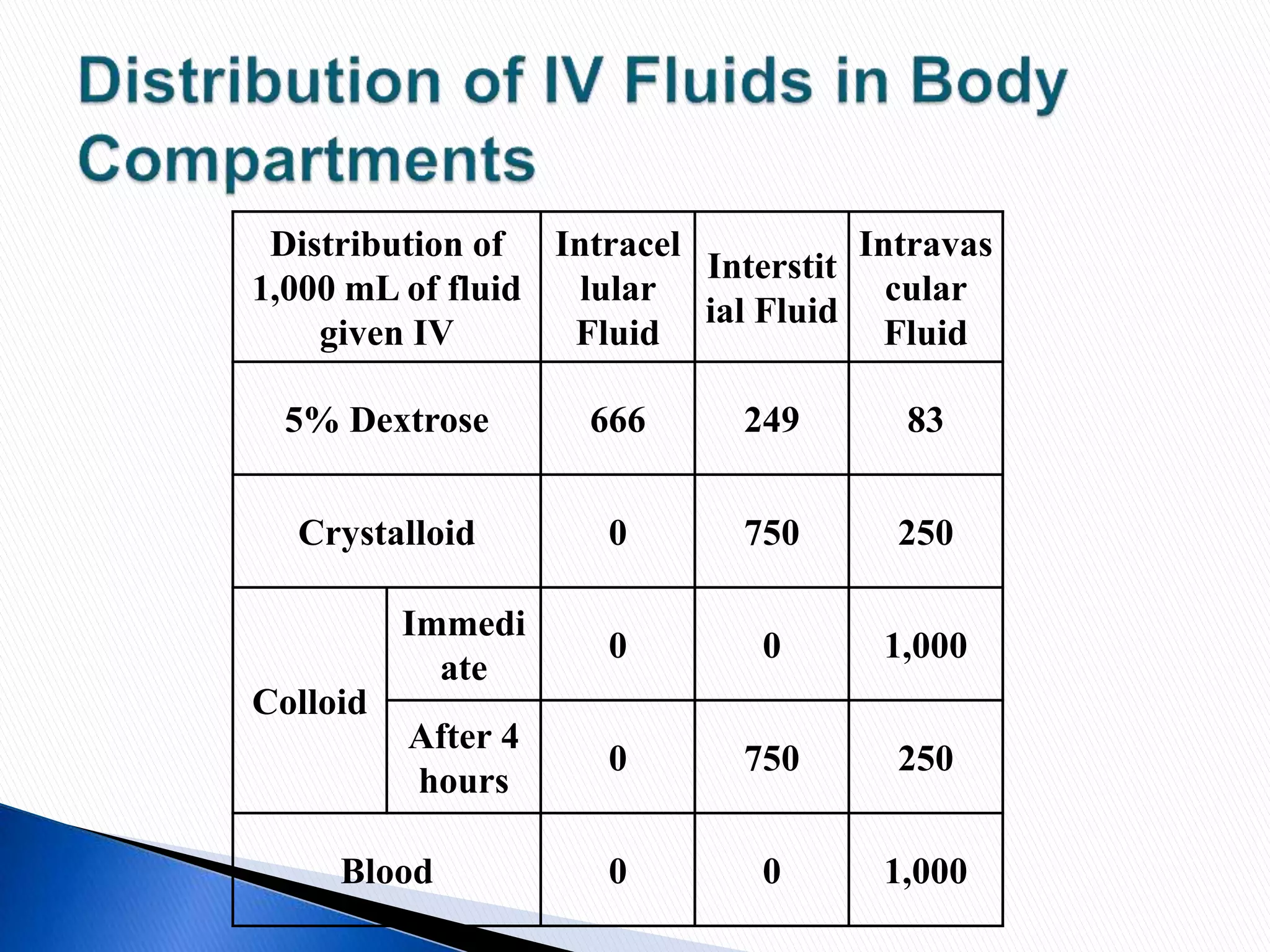
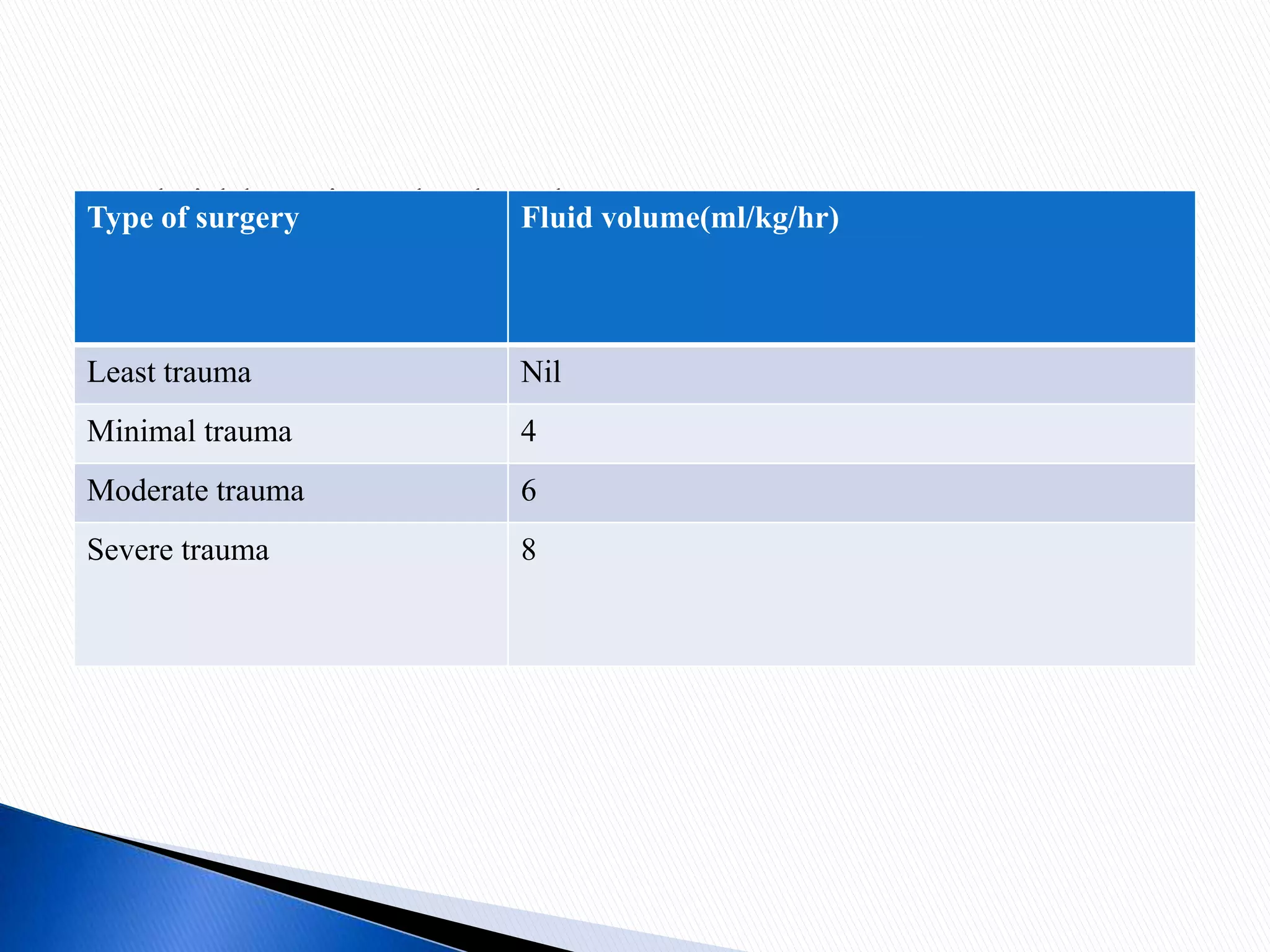
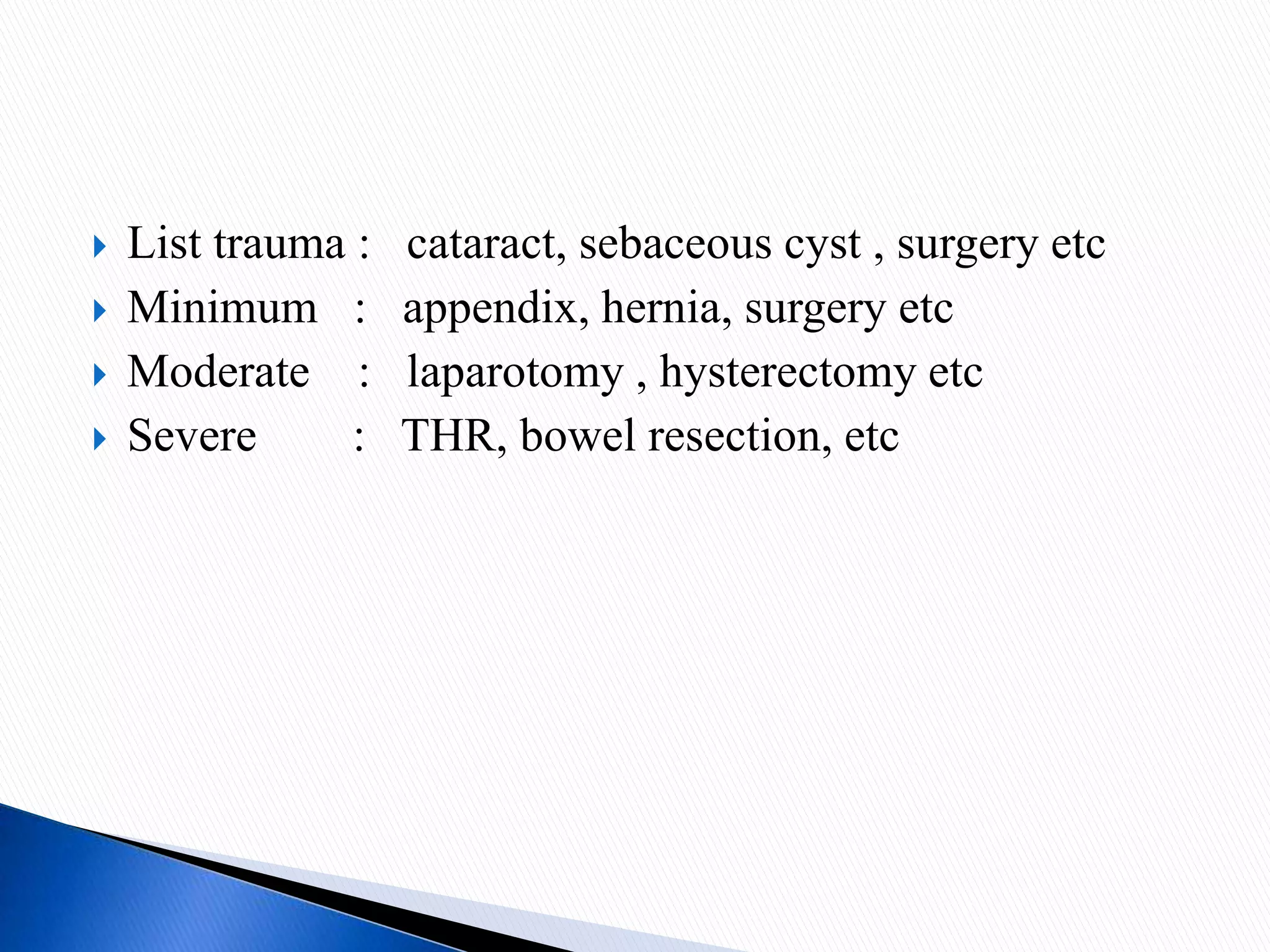
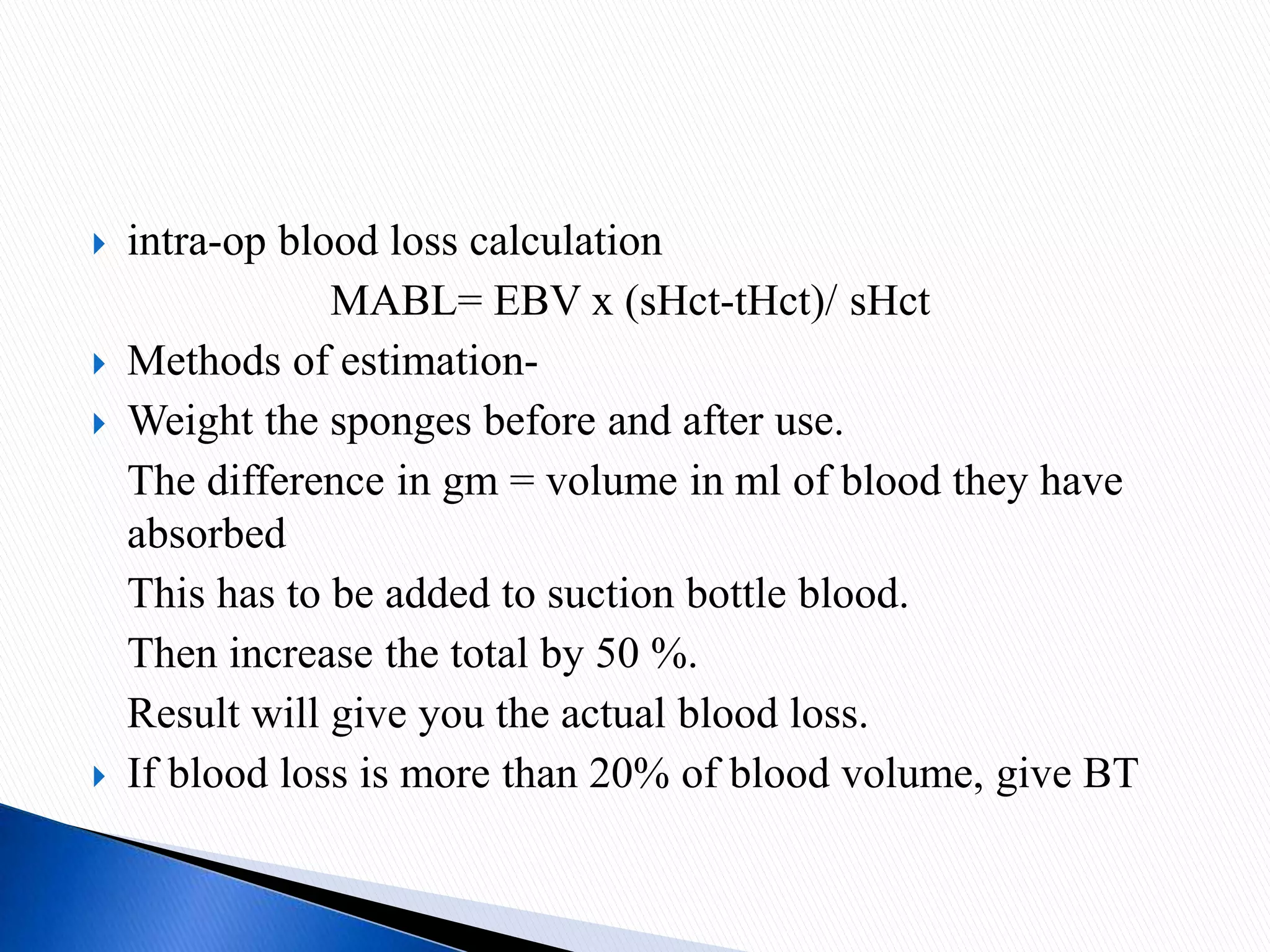
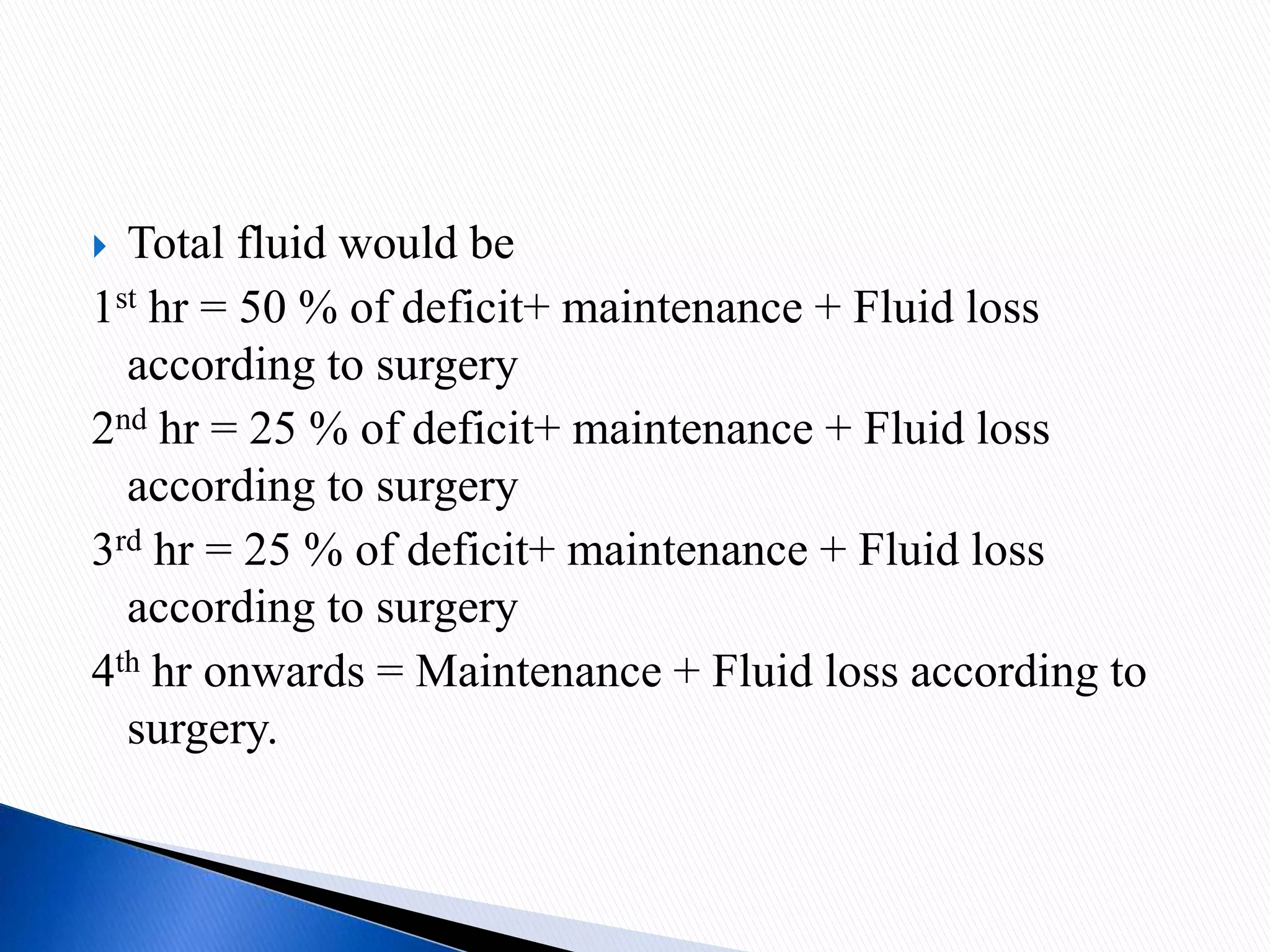
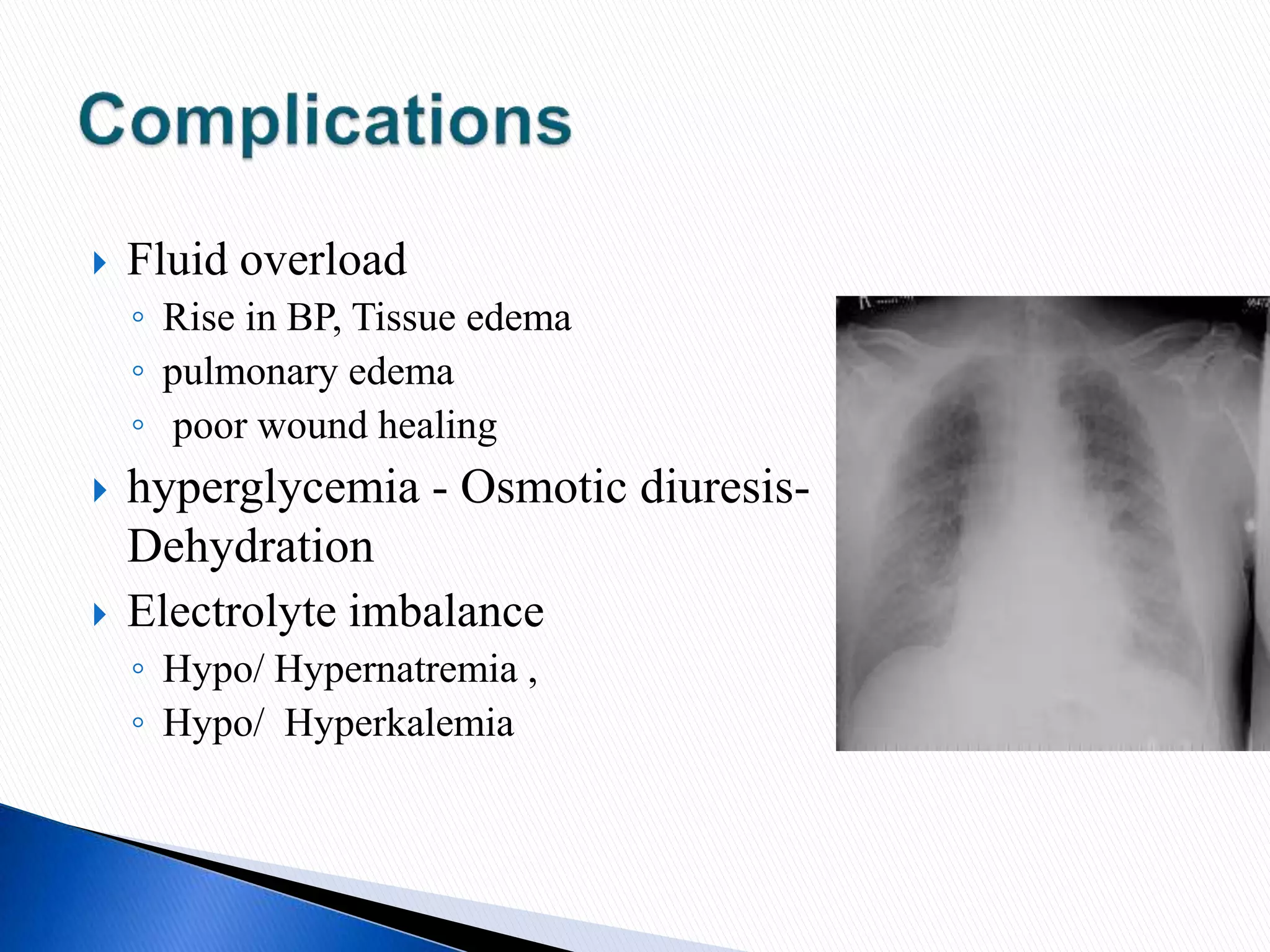
This document discusses the composition and distribution of fluids in the human body. It notes that 60% of the body is fluid, with 40% being intracellular fluid and the remaining extracellular fluid distributed between interstitial fluid and intravascular fluid. It provides details on fluid requirements, losses, electrolyte concentrations in different compartments, and types of intravenous fluids including crystalloids and colloids. The document emphasizes the importance of fluid balance and maintenance of adequate hydration and outlines factors to consider for fluid management in pre-operative, intra-operative, and post-operative settings.