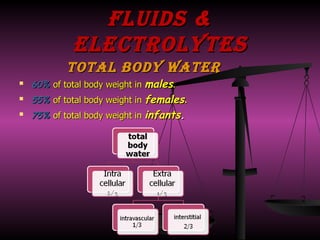
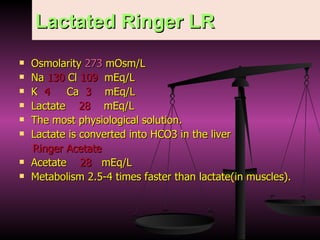
The document discusses fluid and electrolyte therapy under the supervision of Dr. Ashraf Thabet. It covers topics like total body water, water sources and losses, electrolyte metabolism, types of fluids including crystalloids and colloids, and guidelines for perioperative fluid therapy. Clinical signs and treatment of various fluid and electrolyte imbalances like hyponatremia, hypernatremia, hypokalemia, and hypocalcemia are also summarized.































![Acid Base Imbalance I Metabolic Acidosis Causes Over production of organic acid DKA-Lactic acidosis of sepsis and shock [ HIGH ANION GAP ] Renal failure(acute-chronic) Excessive loss of HCO3(diarrhea,pancreatic or small intestinal fistula,uretro sigmoidostmy [ NORMAL ANION GAP ] C/P increased rate&depth of breathing TTT mild to moderate ttt of cause Sever (IV HCO3 causes (1/2body weight X (15-HCO3))](https://image.slidesharecdn.com/fluids-electrolytes-1287179914-phpapp02/85/Fluids-Electrolytes-39-320.jpg)

