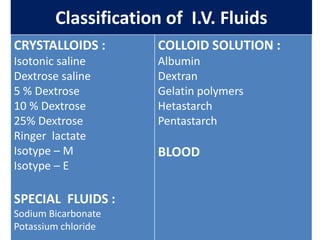
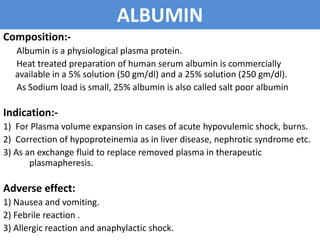
1) The document discusses various intravenous fluid options including crystalloids like normal saline, Ringer's lactate, dextrose saline and colloids like albumin and dextran.
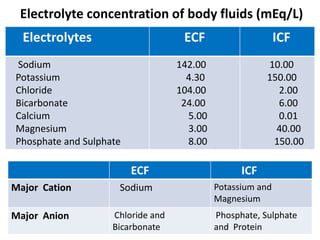
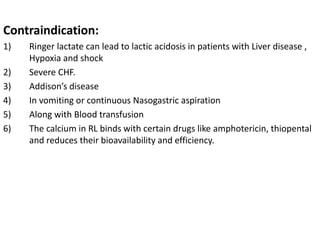
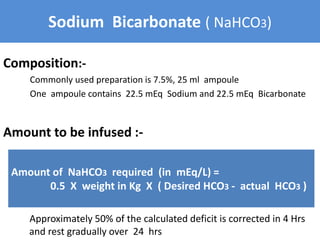
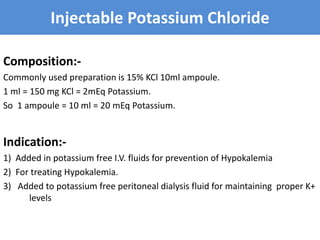
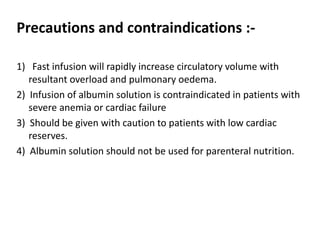
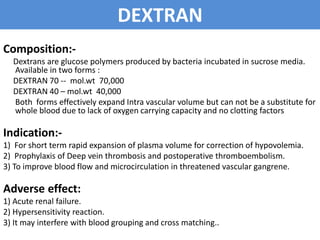
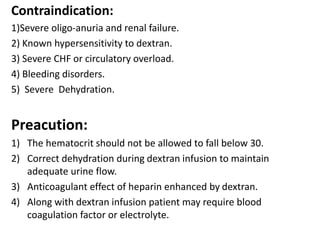
2) It provides the composition, indications, contraindications and precautions for each fluid. Daily fluid balance and electrolyte concentrations in body fluids are also reviewed.
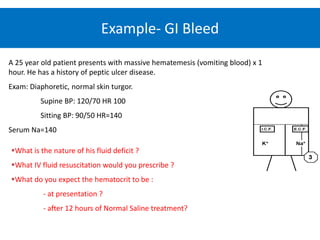
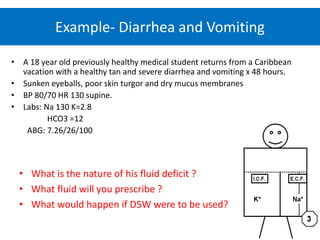
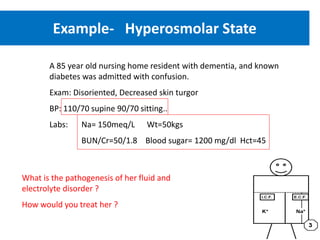
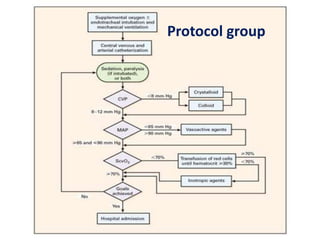
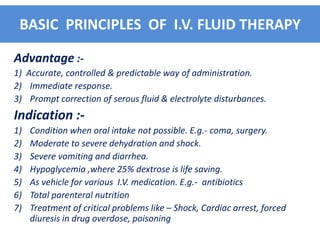
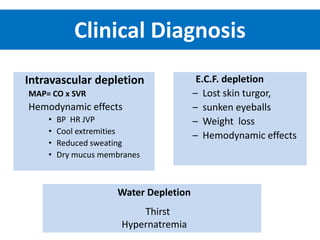
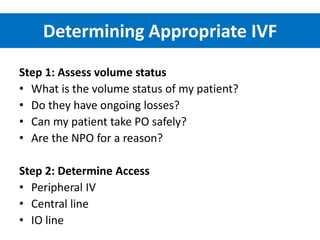
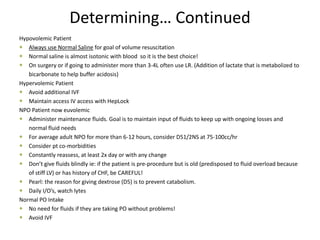
3) Calculating plasma osmolality and basic principles of IV fluid therapy including advantages, disadvantages, classification and complications are summarized. Clinical examples of fluid depletion and specific treatment approaches are mentioned.





















![Calculating Drip Rate
In the age of machines, we barely have to do this
anymore… but if you ever need to go old skool, here is
how to calculate the drip rate (drops/minute):
gtt = Volume to be infused (mL) x (gtt/mL)
min Time (minutes)
Drip Factor = (gtt/mL) Of the TUBING which is found on the
manufacturers pacakging
Example: Volume = 4000 ml
Time = 24 hours
Drip factor of tubing = 15 gtt/ml.
So…. [4000mL/(24h x 60min/h)] X 15gtt/ml = approx 42 drops/min](https://image.slidesharecdn.com/dailyfluidbalance-151108100439-lva1-app6892/85/Daily-fluid-balance-40-320.jpg)