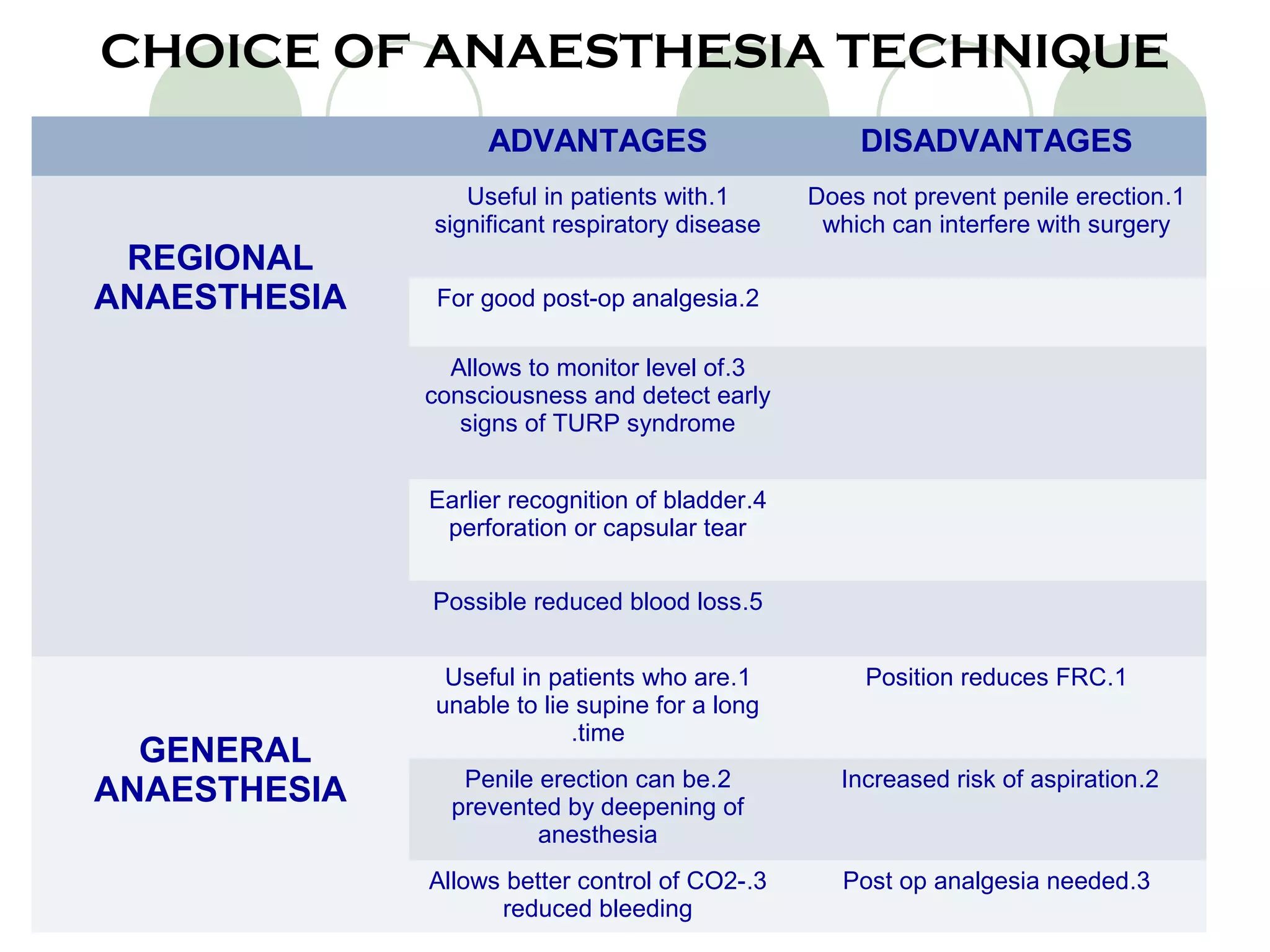
TURP is a procedure to relieve urinary symptoms from an enlarged prostate. It carries risks due to the elderly patient population and long duration. A thorough pre-op assessment helps determine anesthesia technique, with subarachnoid block preferred. Potential complications include hypotension, hemorrhage, bladder perforation, hypothermia, and the rare but serious TURP syndrome caused by excessive fluid absorption. Close monitoring is needed to rapidly identify and treat any issues.