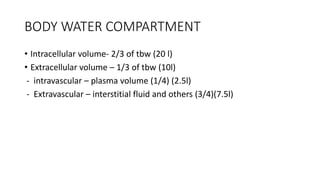
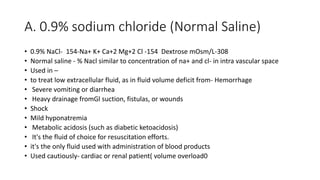
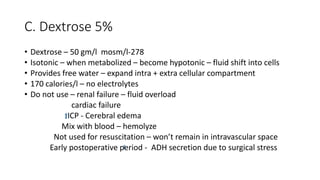
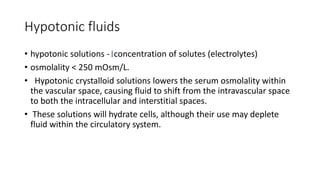
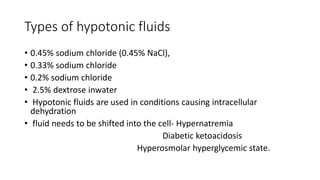
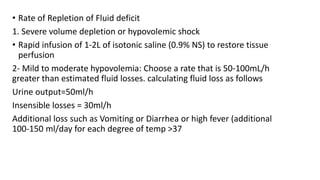
This document discusses intravenous (IV) fluids, including their composition and uses. It covers the different fluid compartments in the body and variations that can occur. Various IV fluid types - isotonic, hypotonic, hypertonic and colloids - are described along with their indications, precautions, and how they alter fluid balance. Factors influencing fluid requirements and principles of fluid therapy for resuscitation, maintenance and replacement are outlined. Signs of overhydration and approaches to manage fluid overload are also summarized.