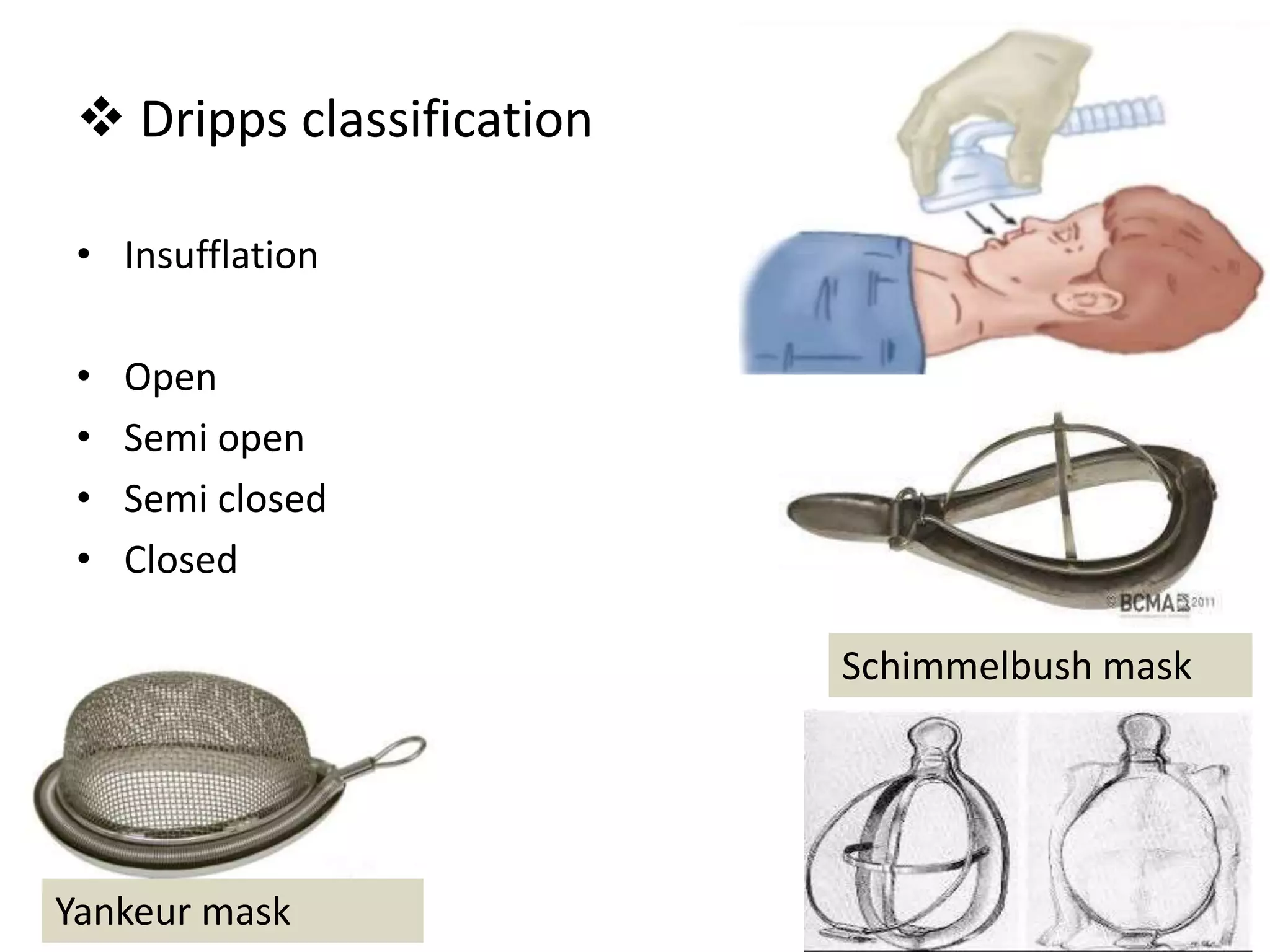
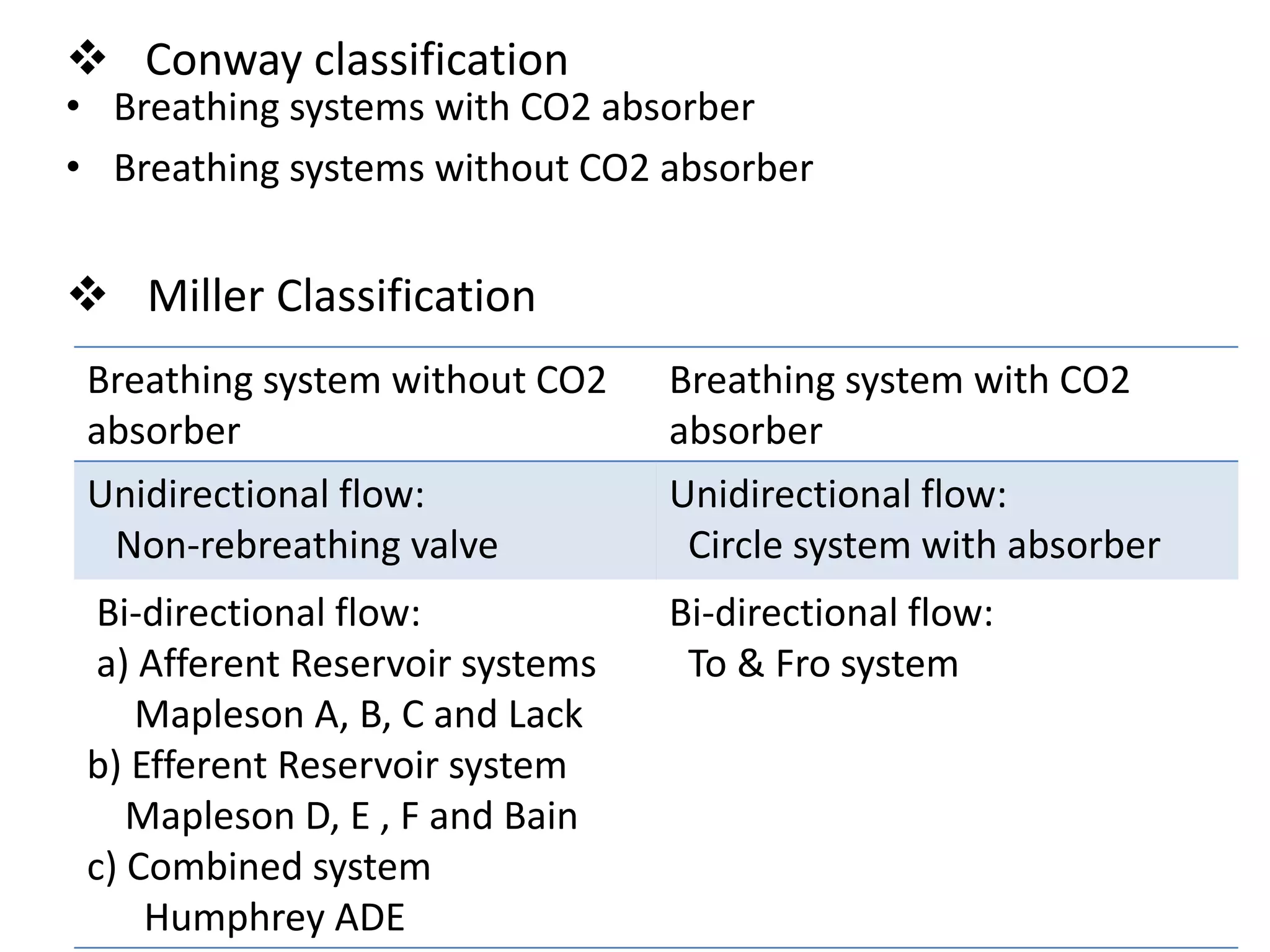
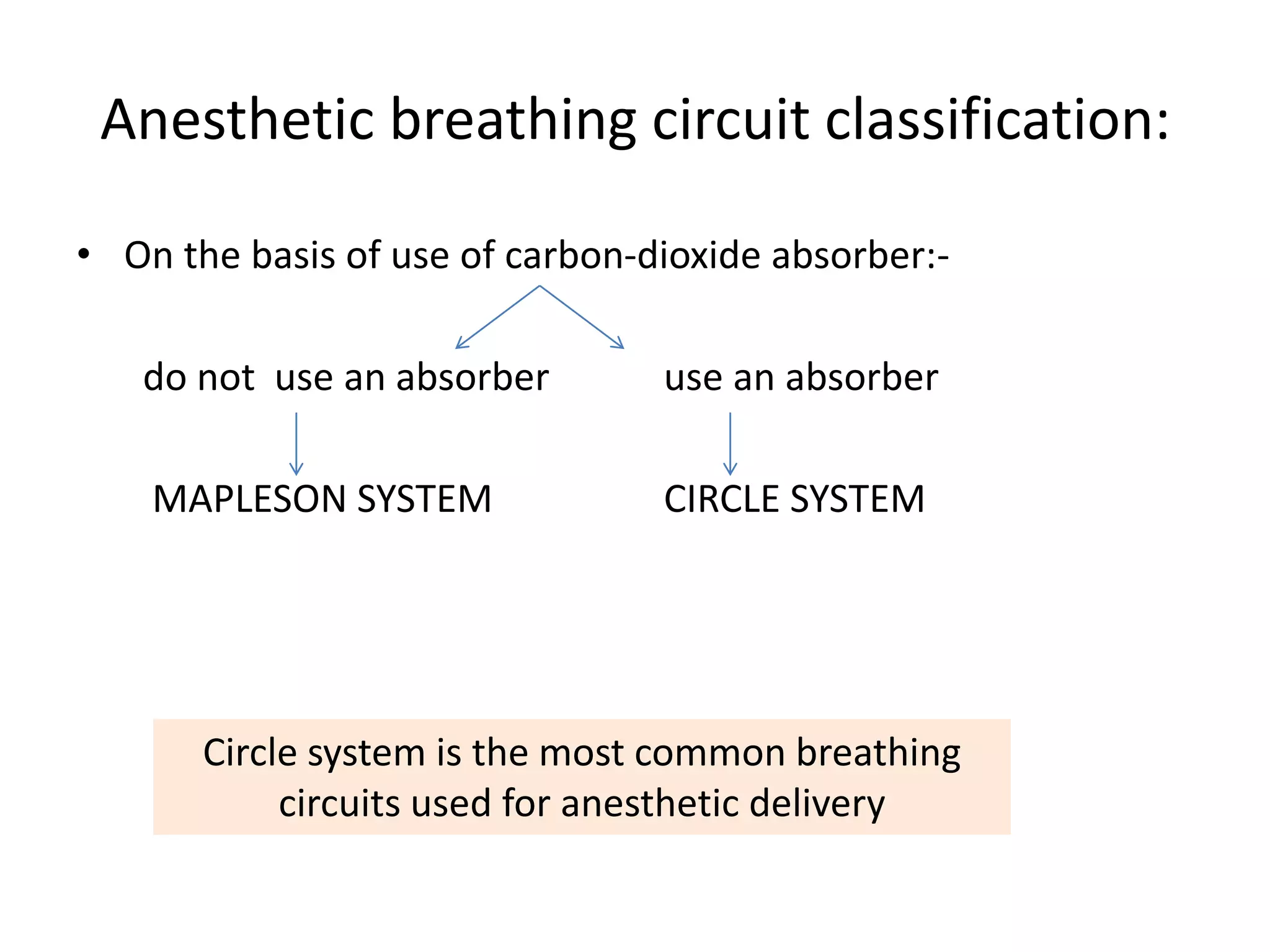
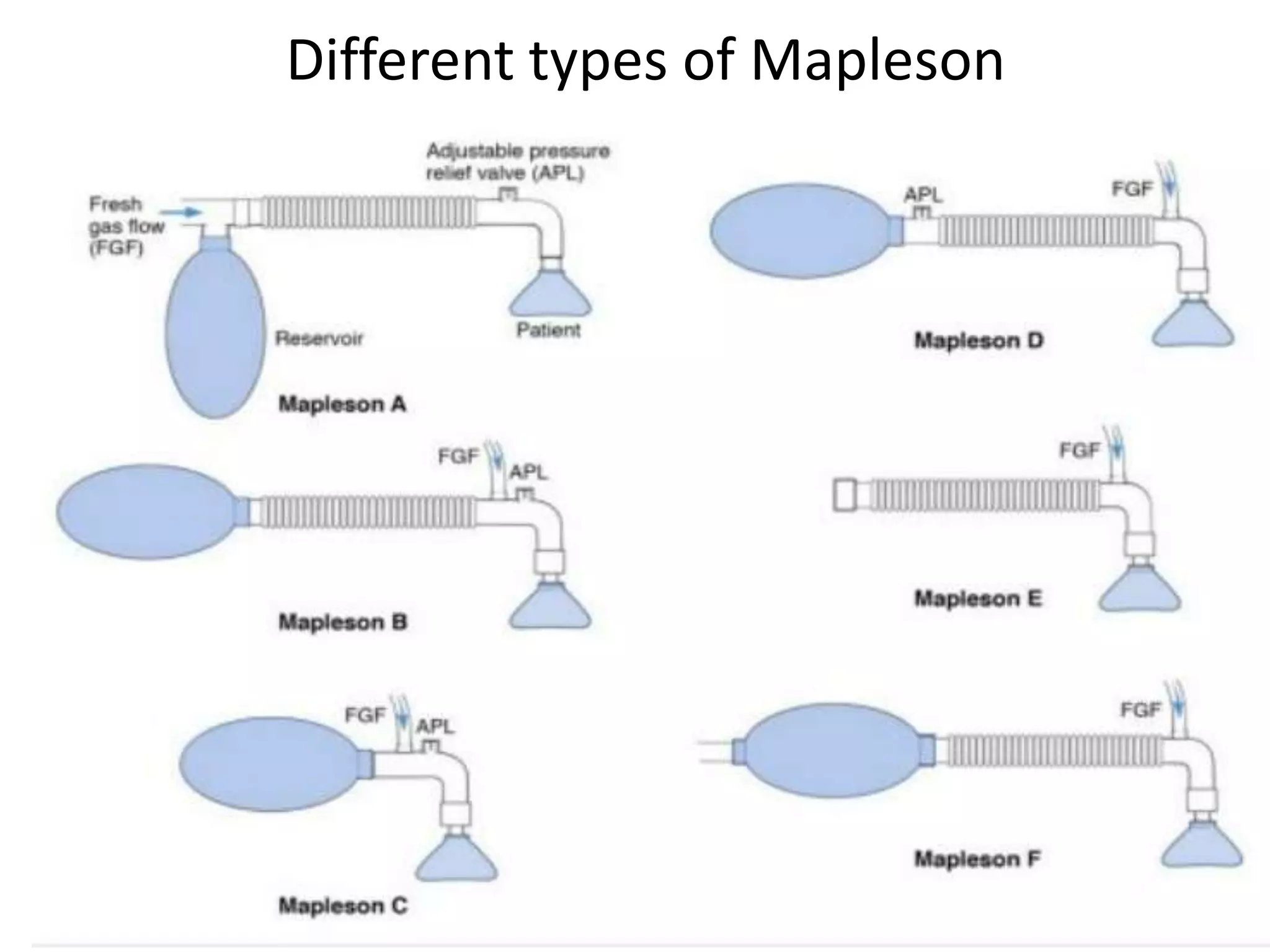
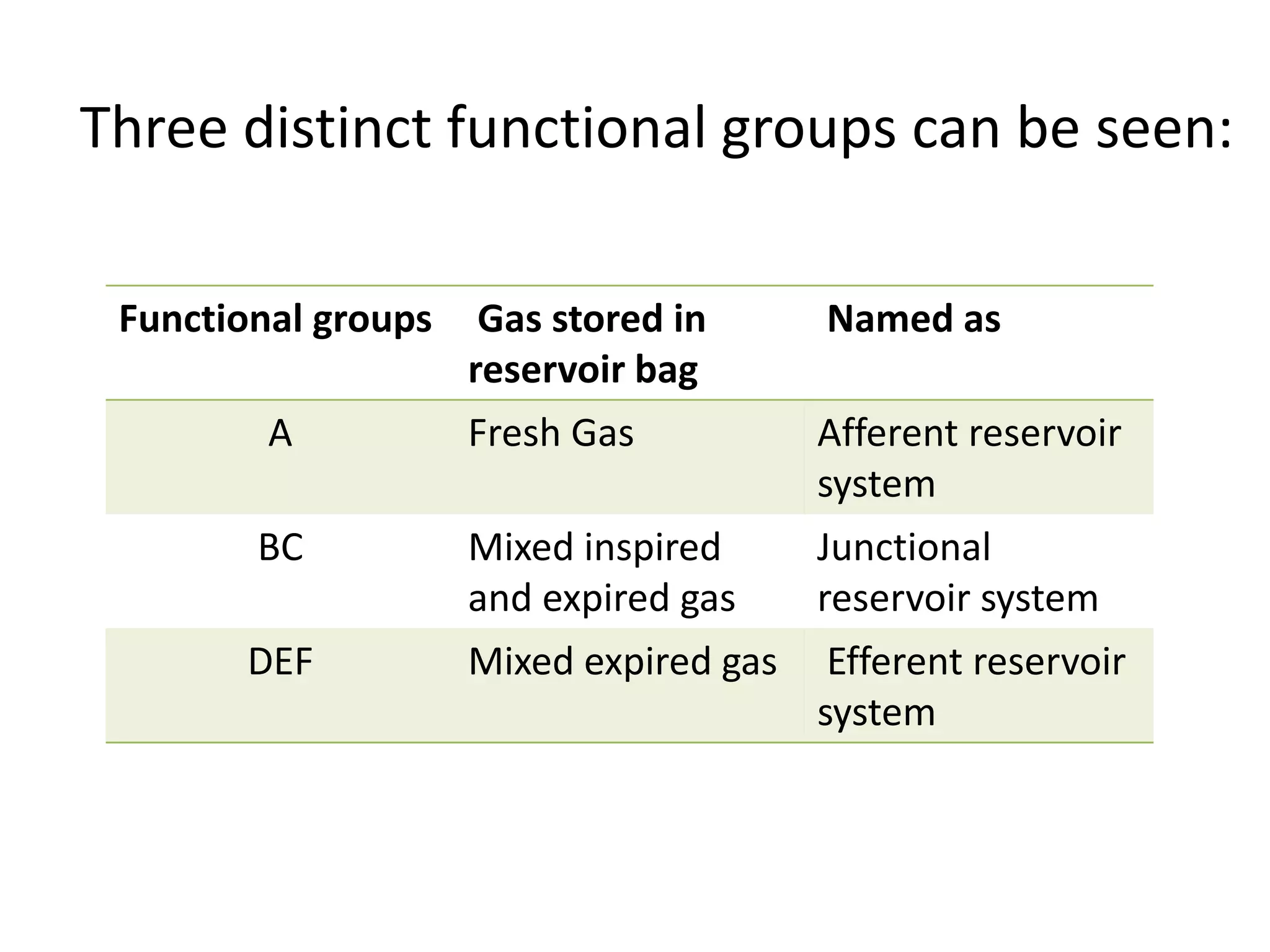
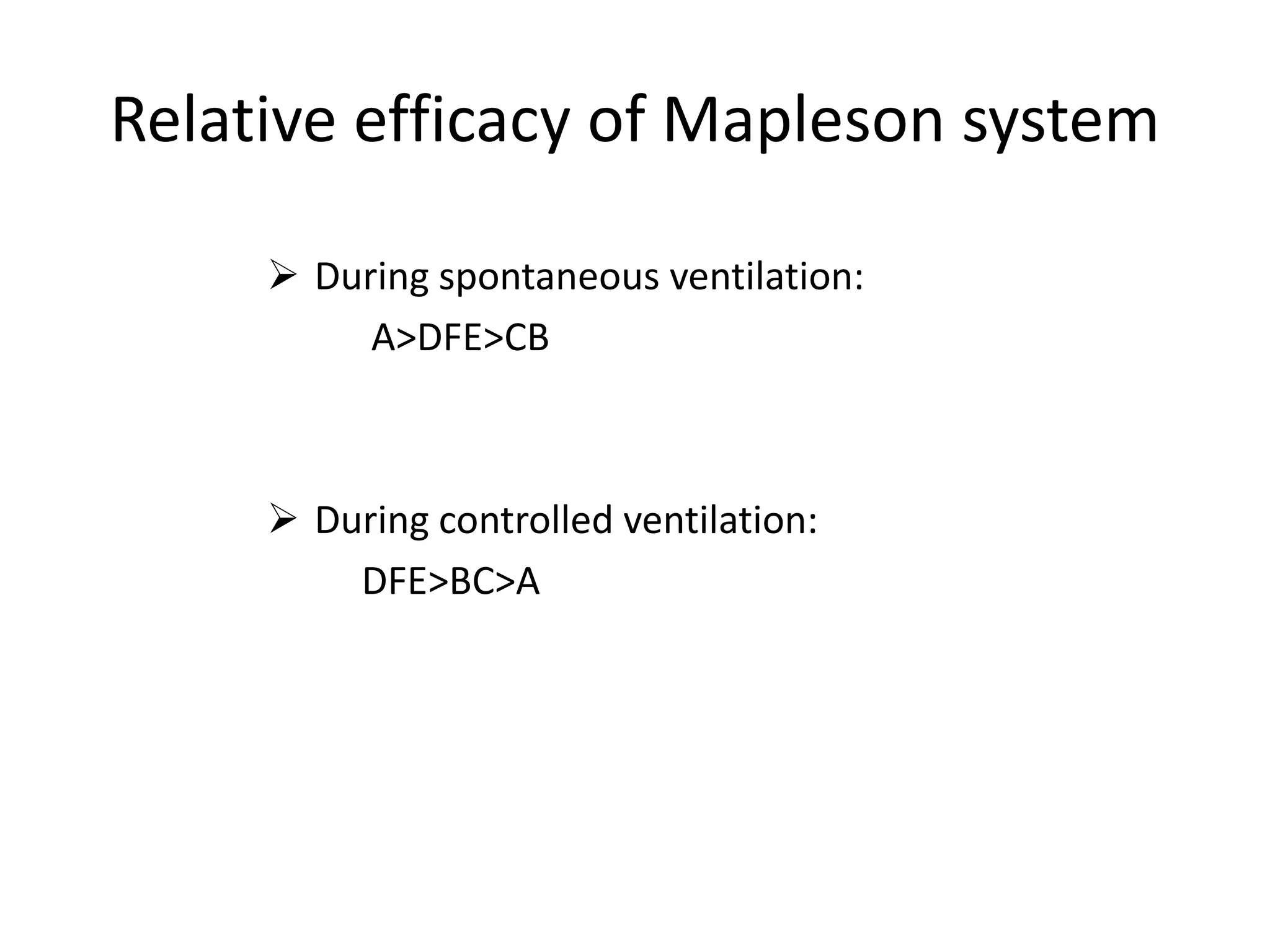
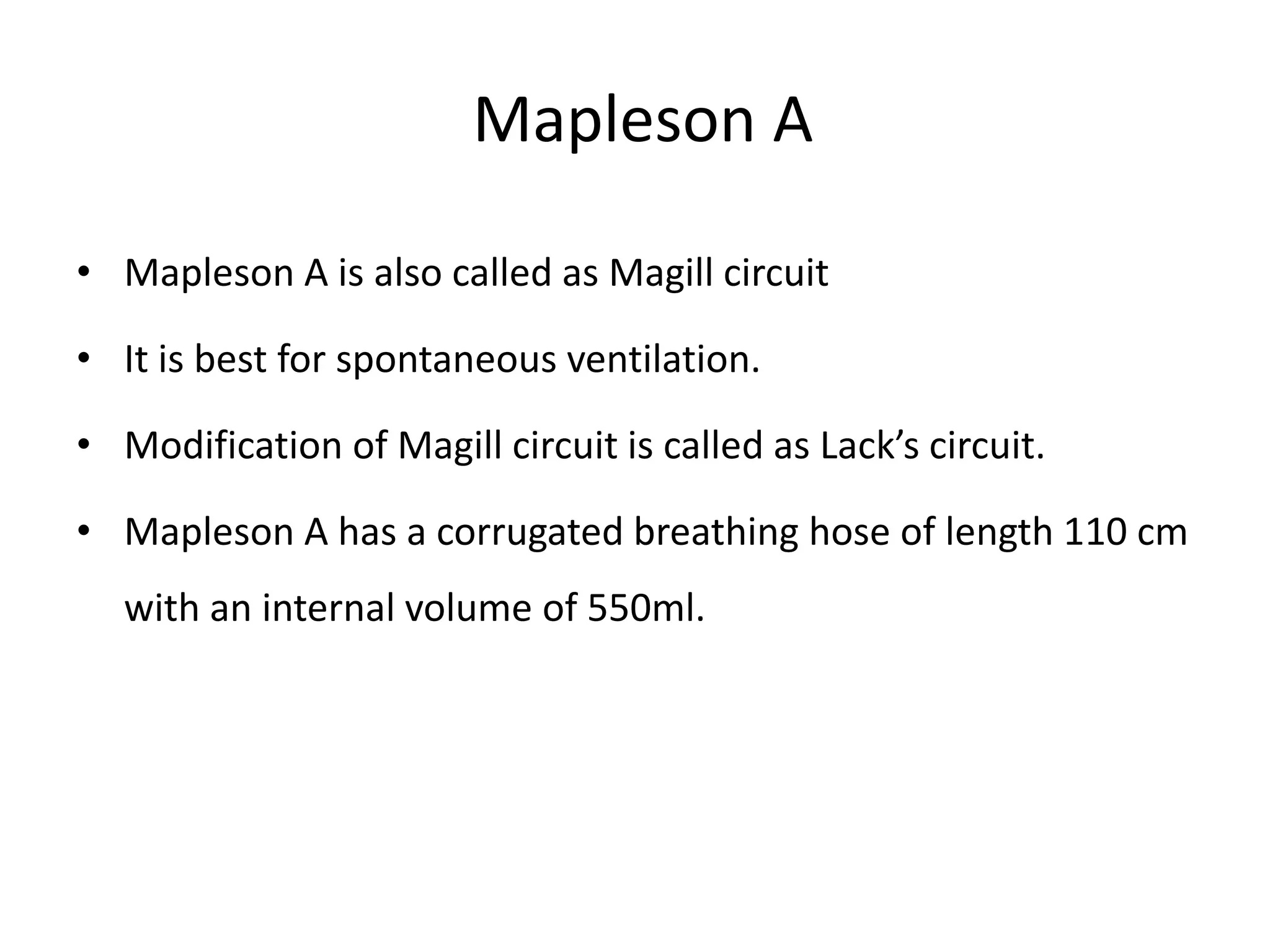
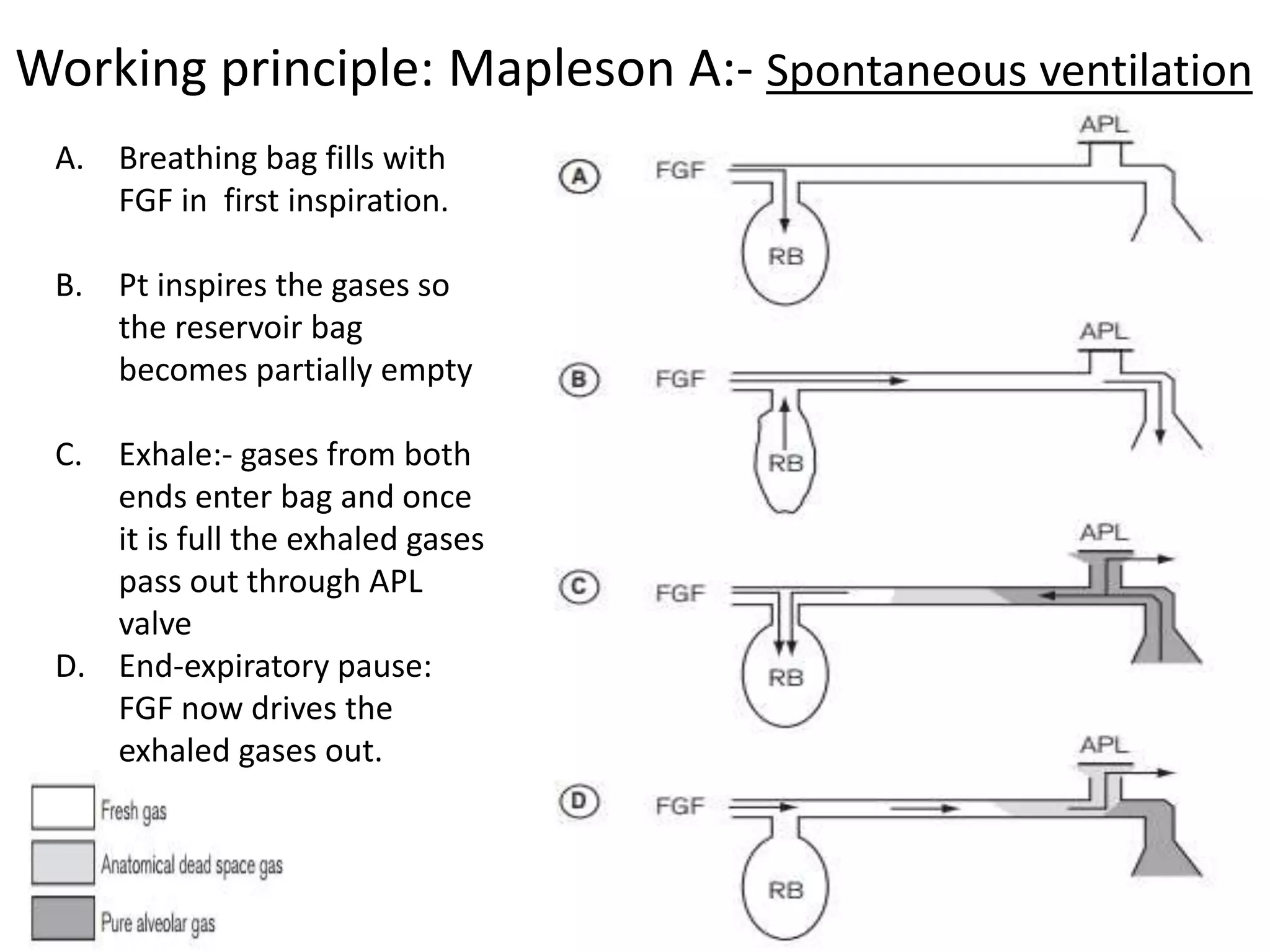
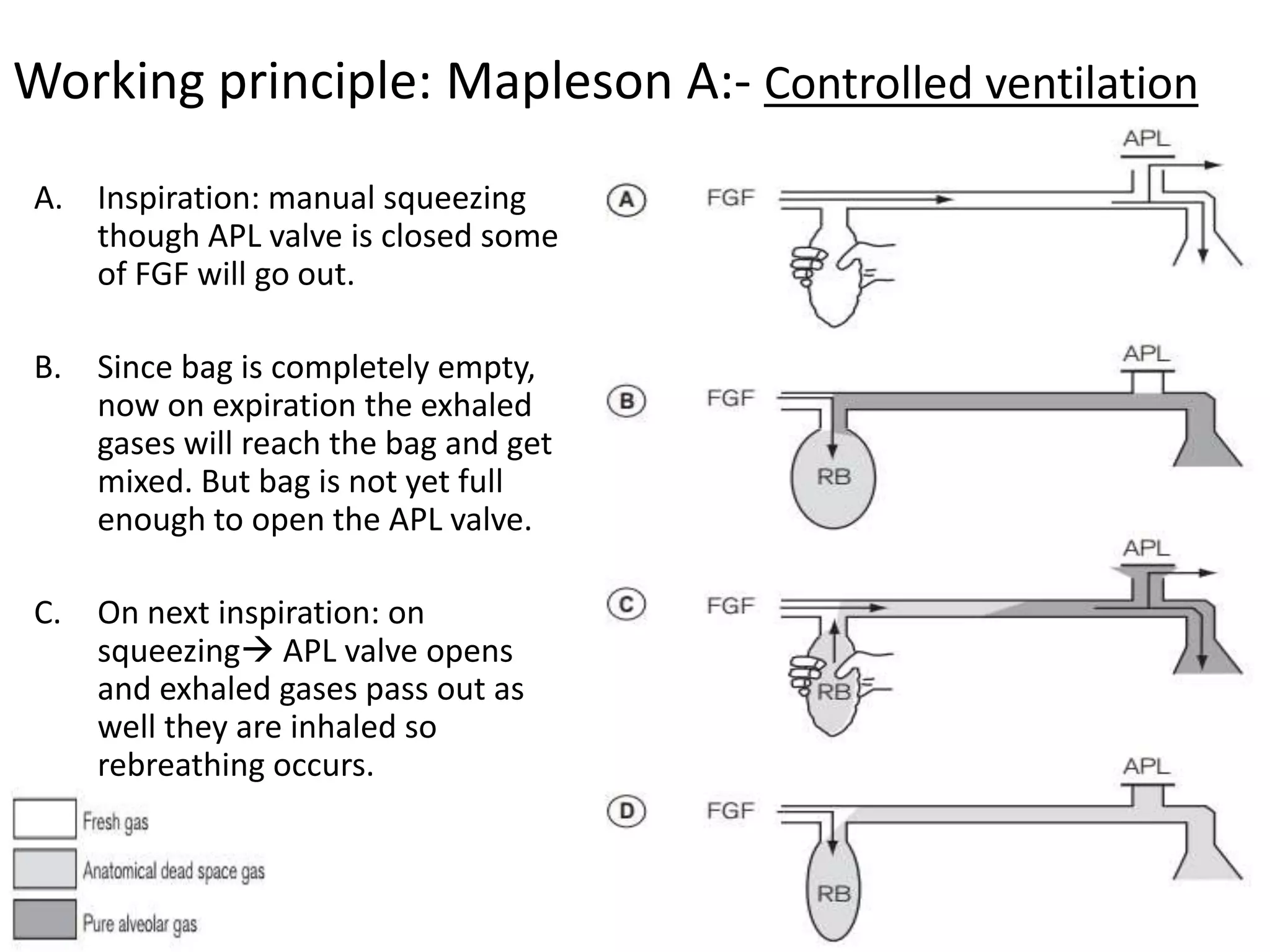
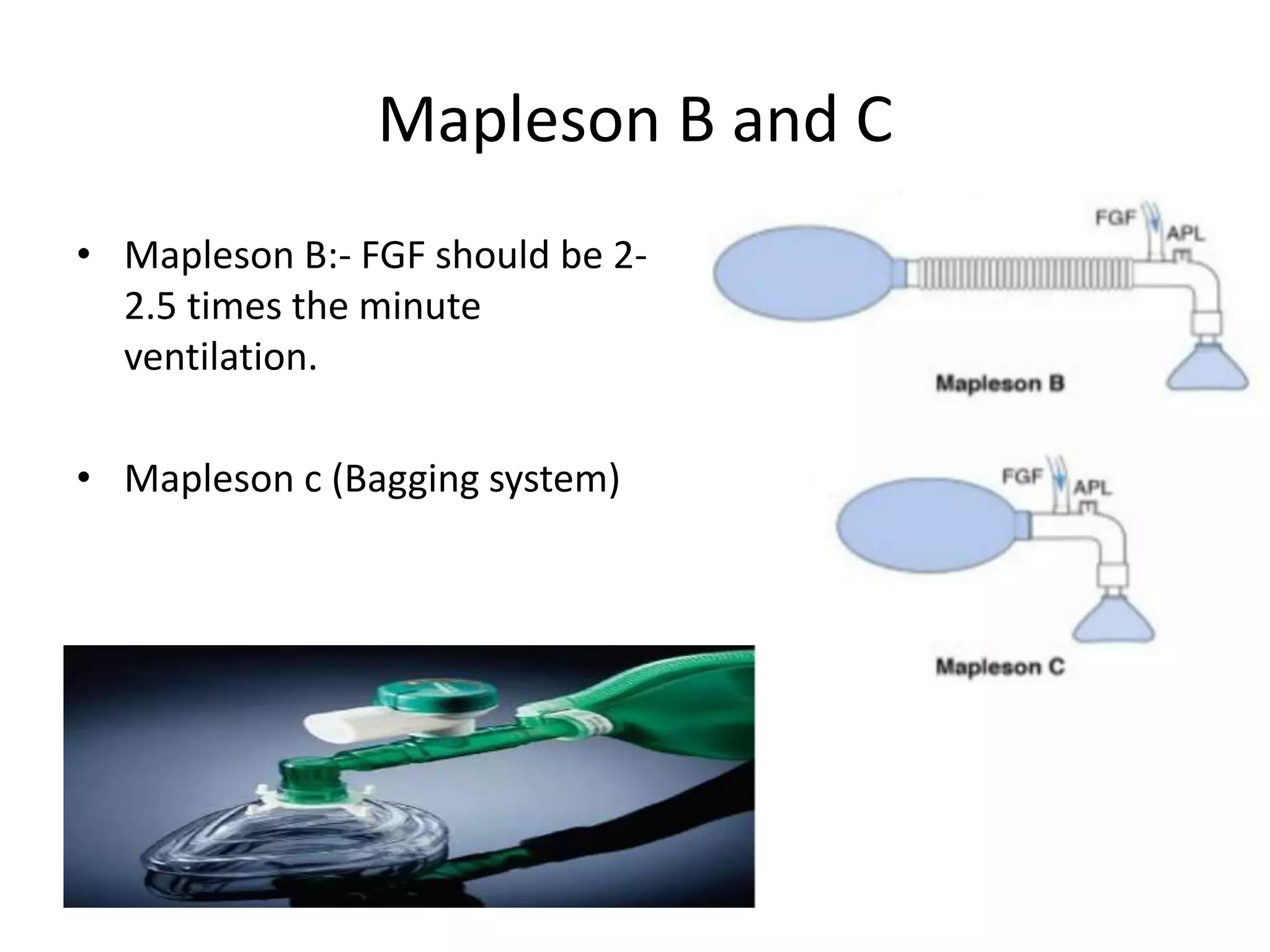
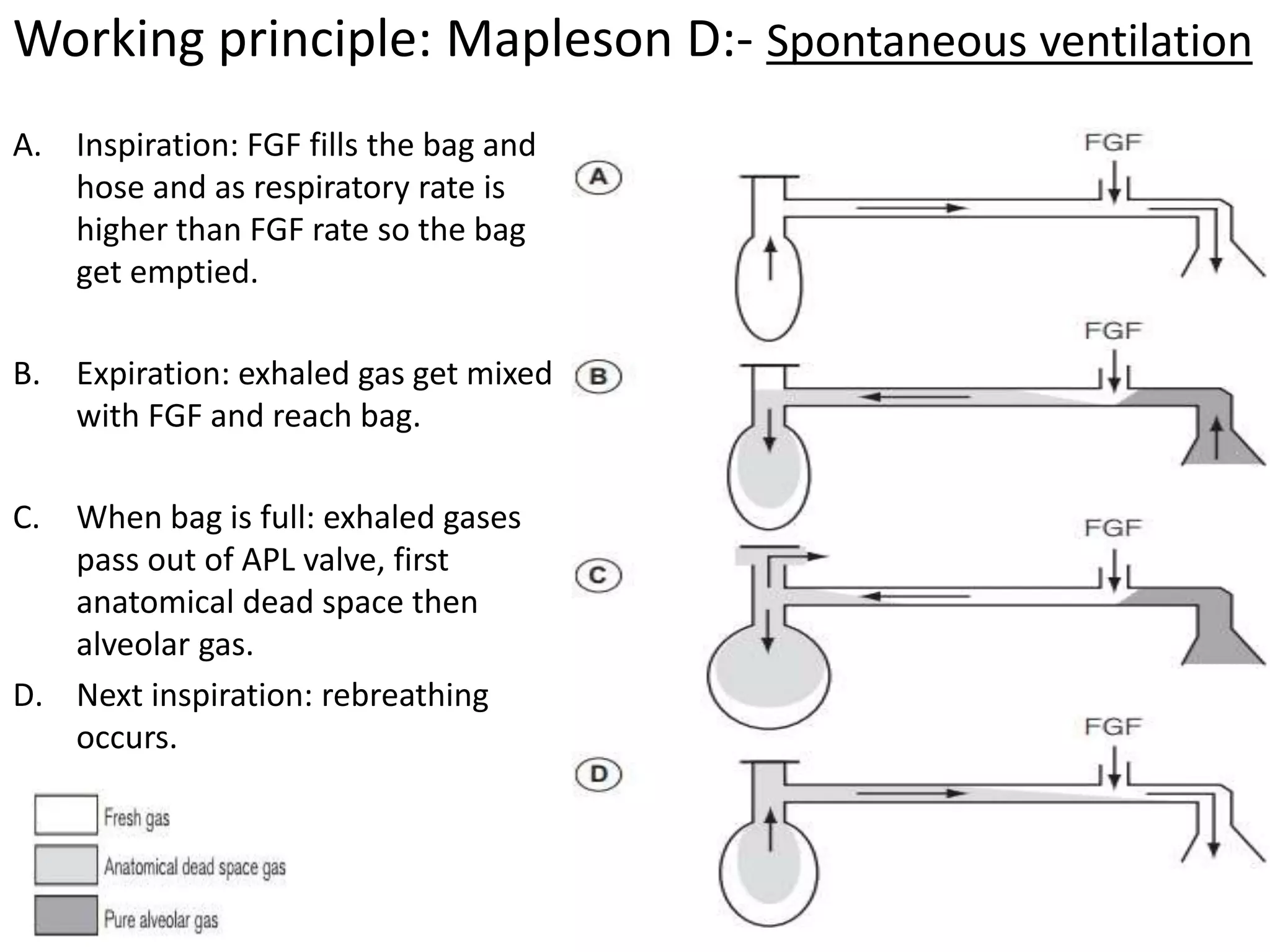
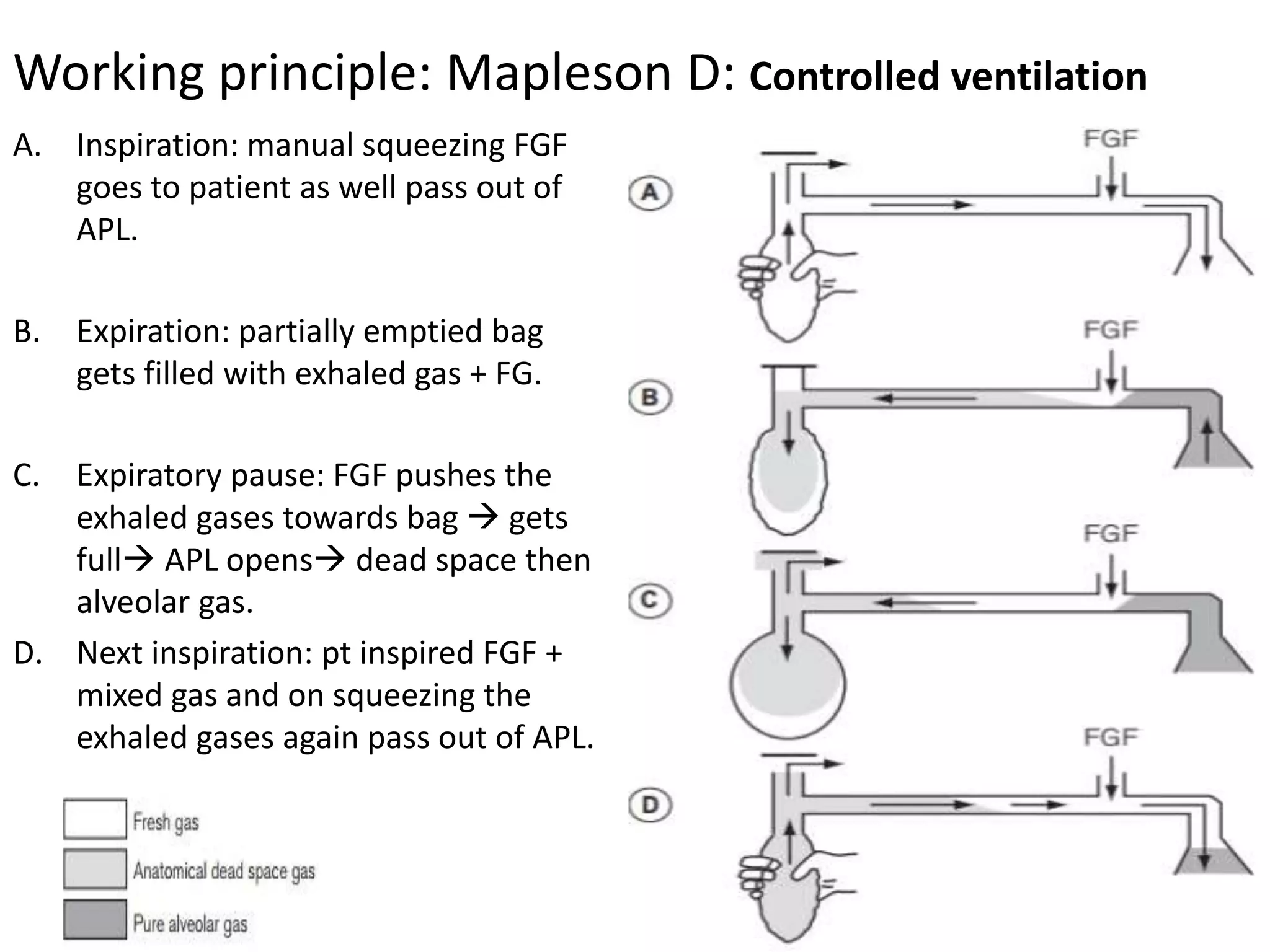
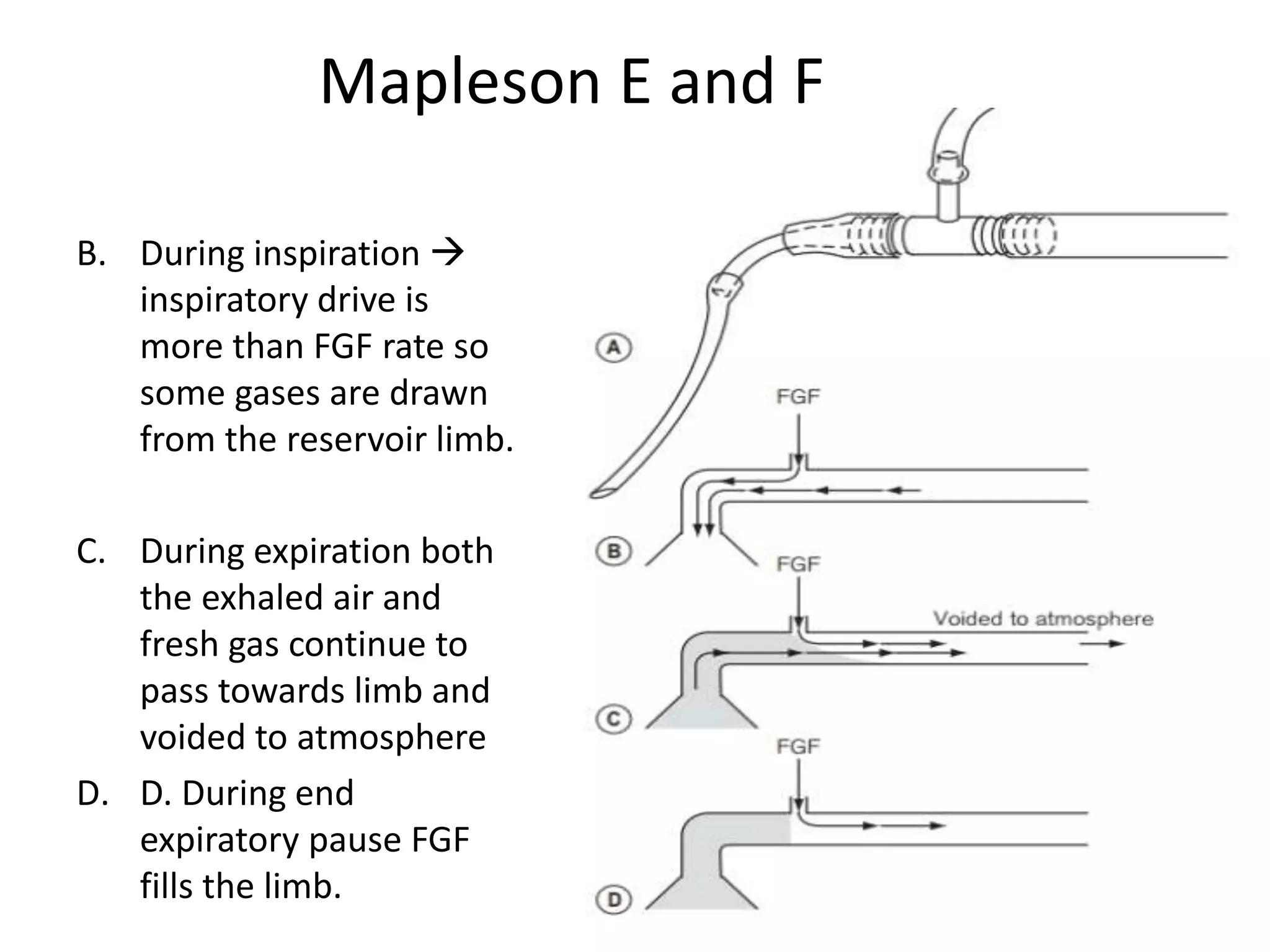
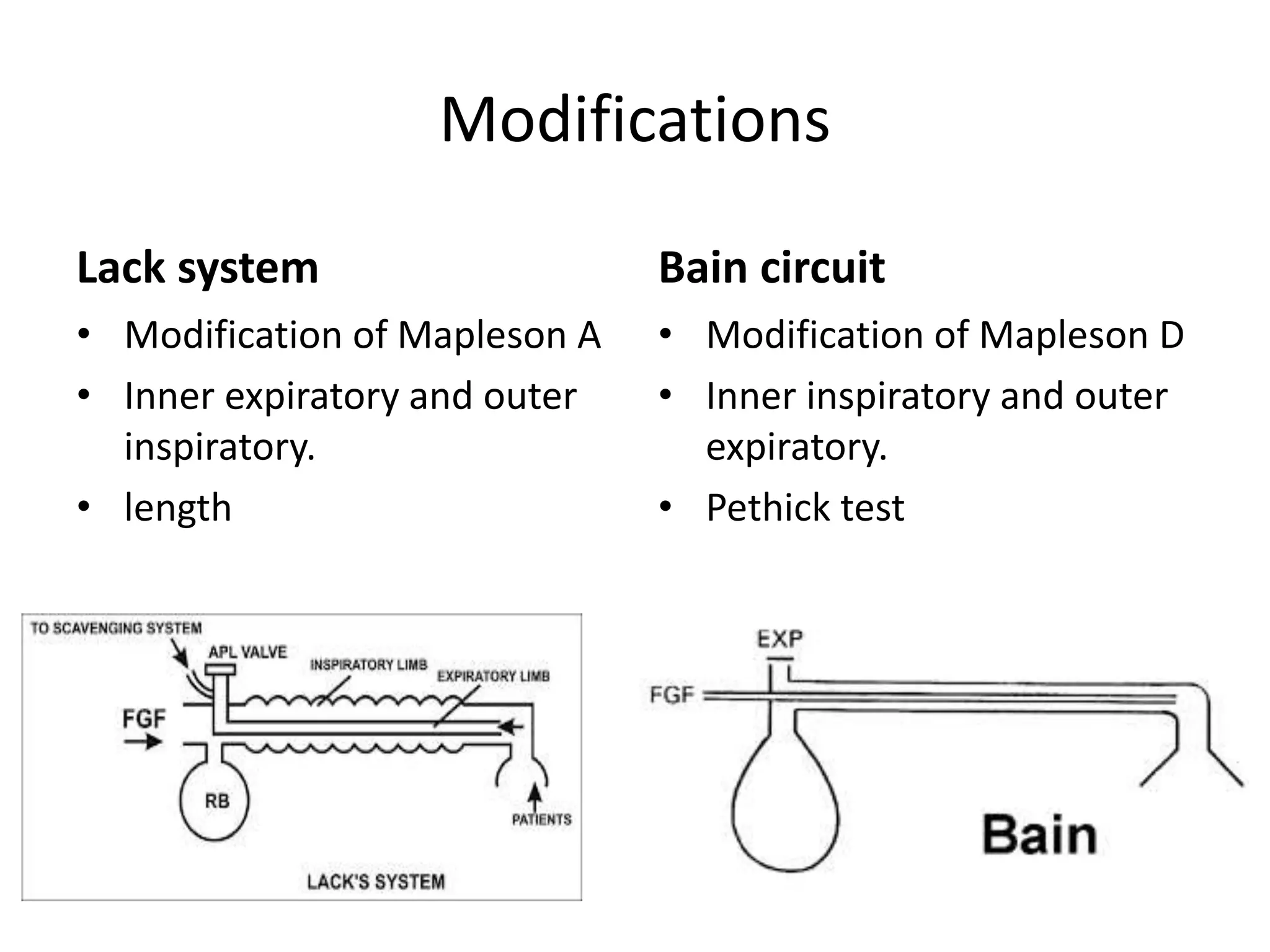
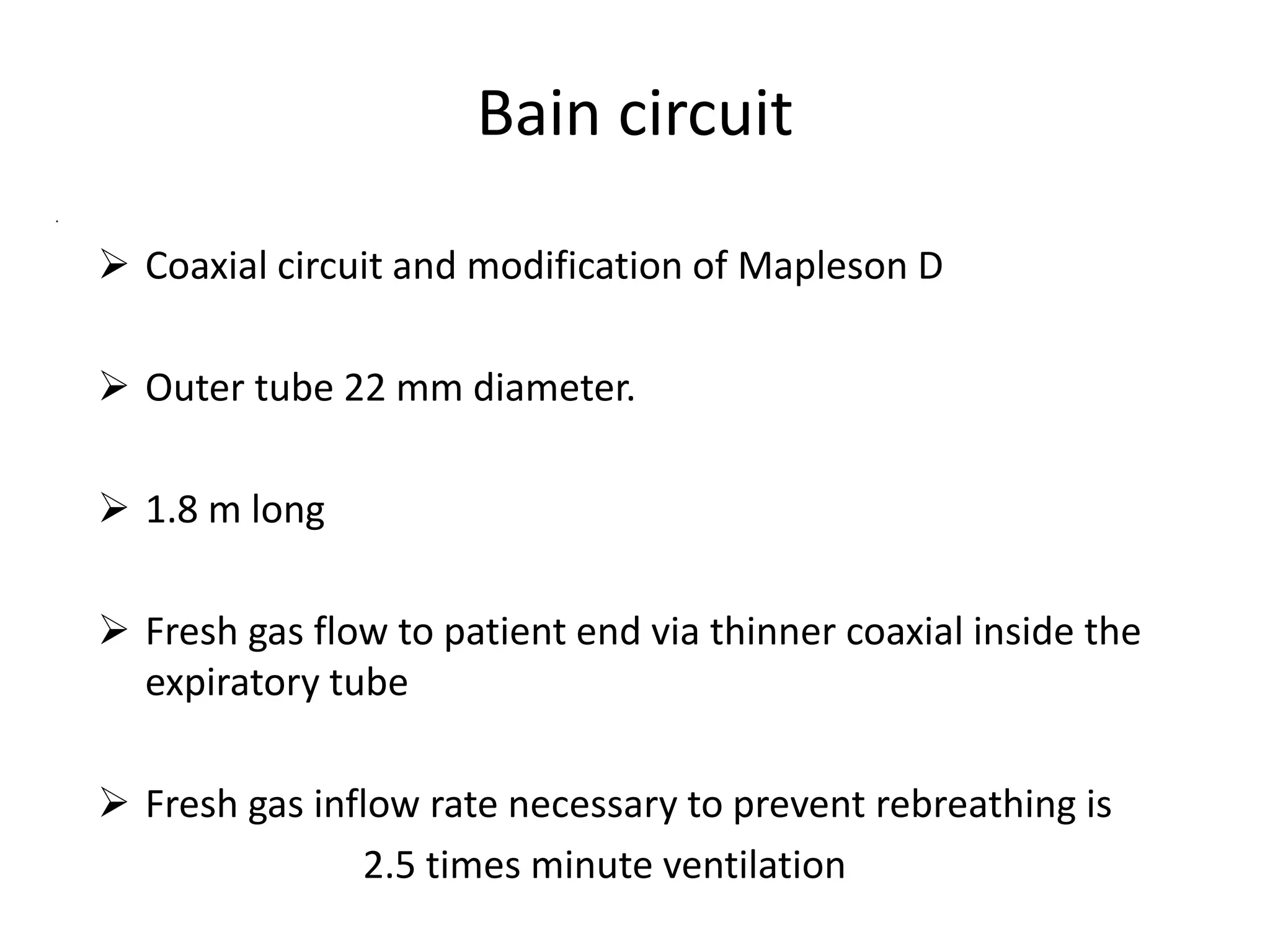
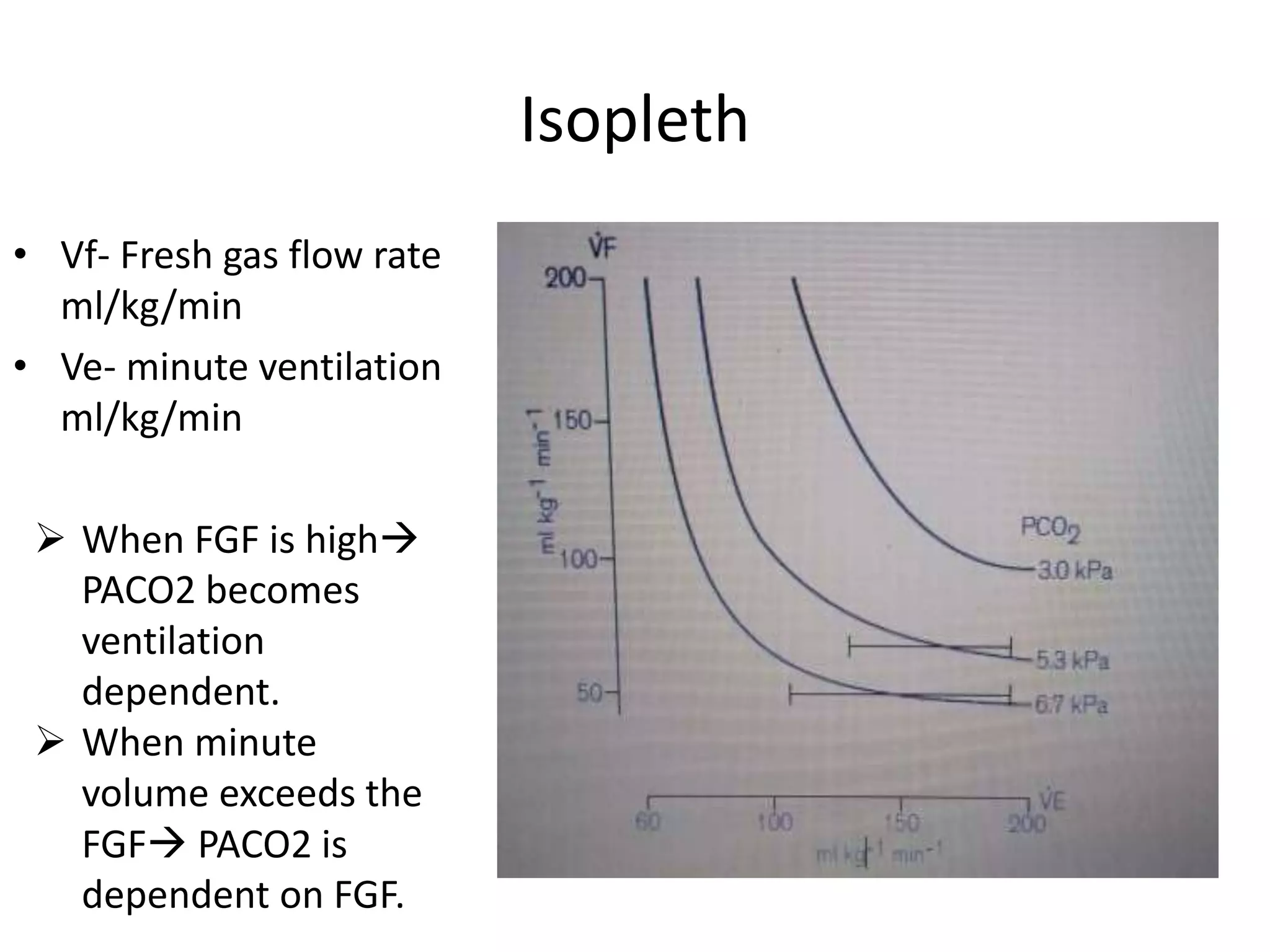
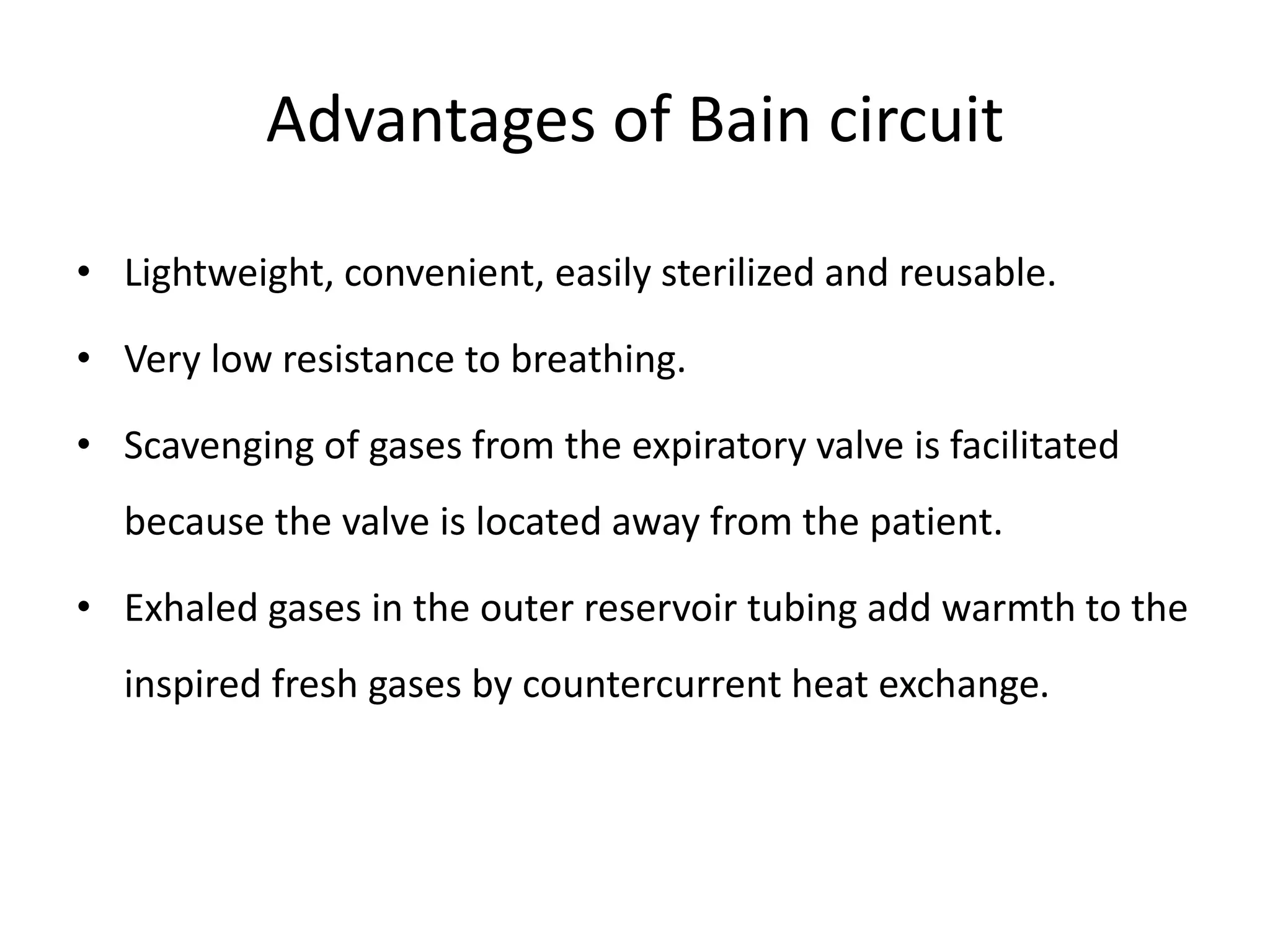
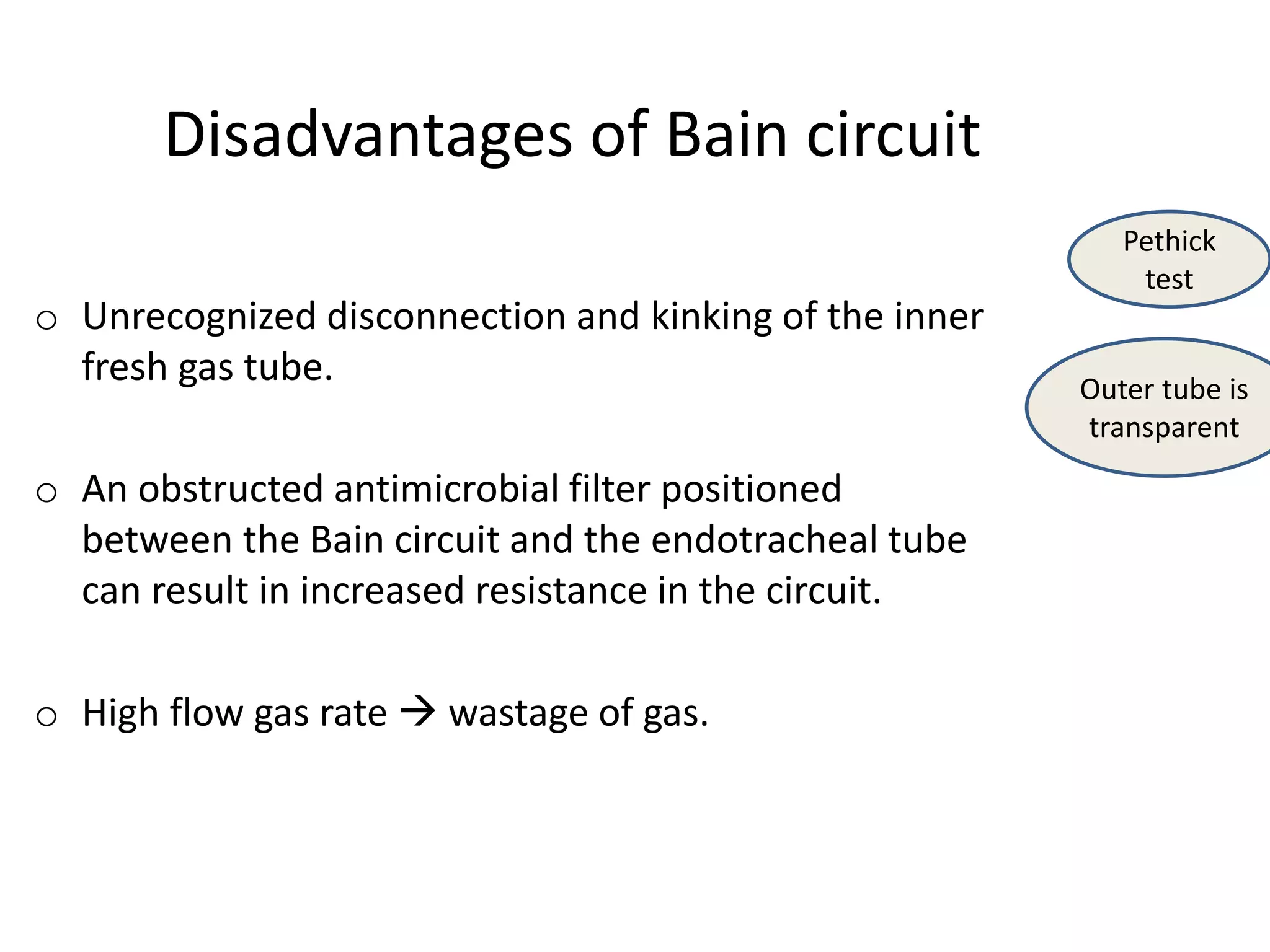
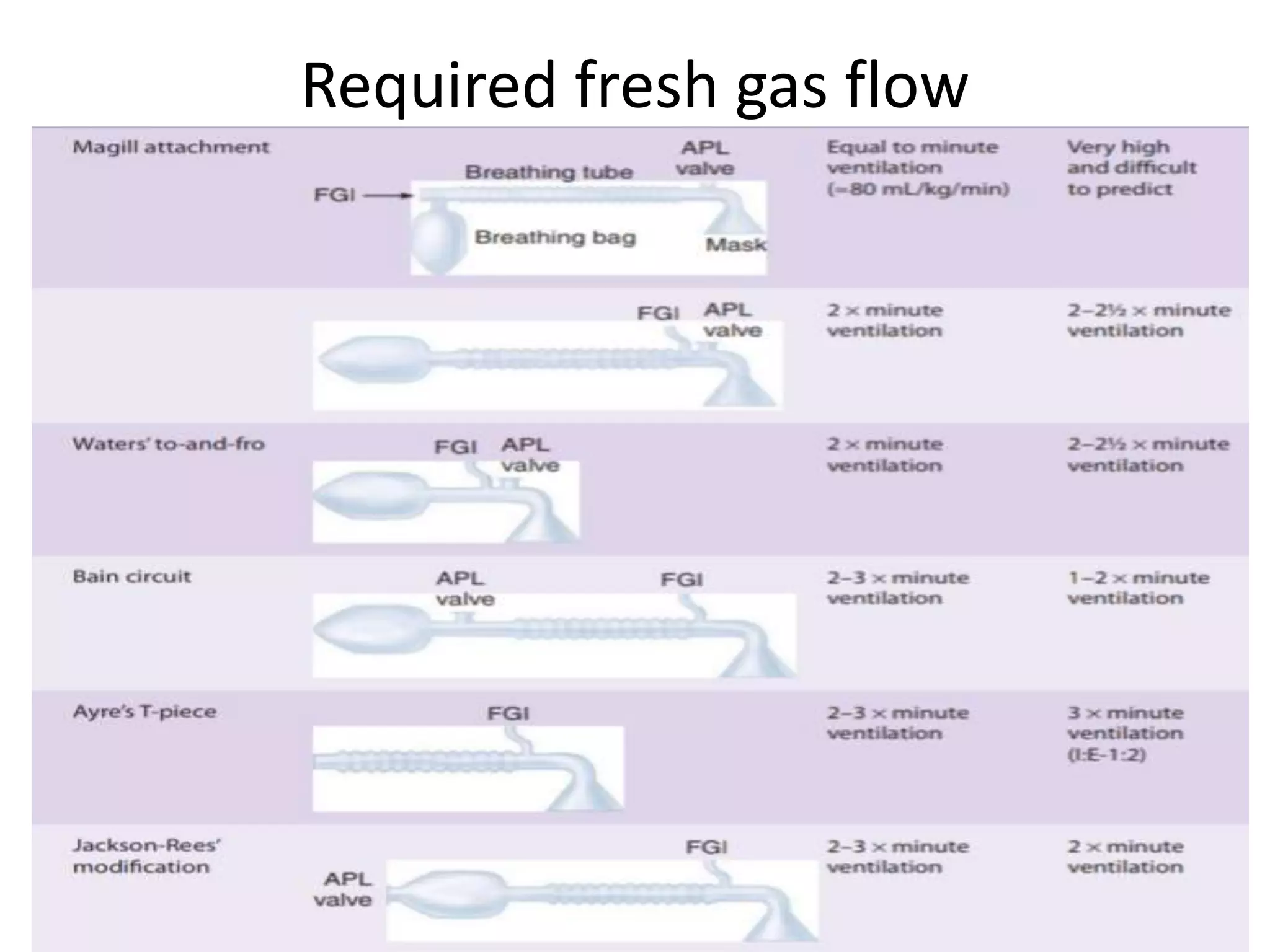
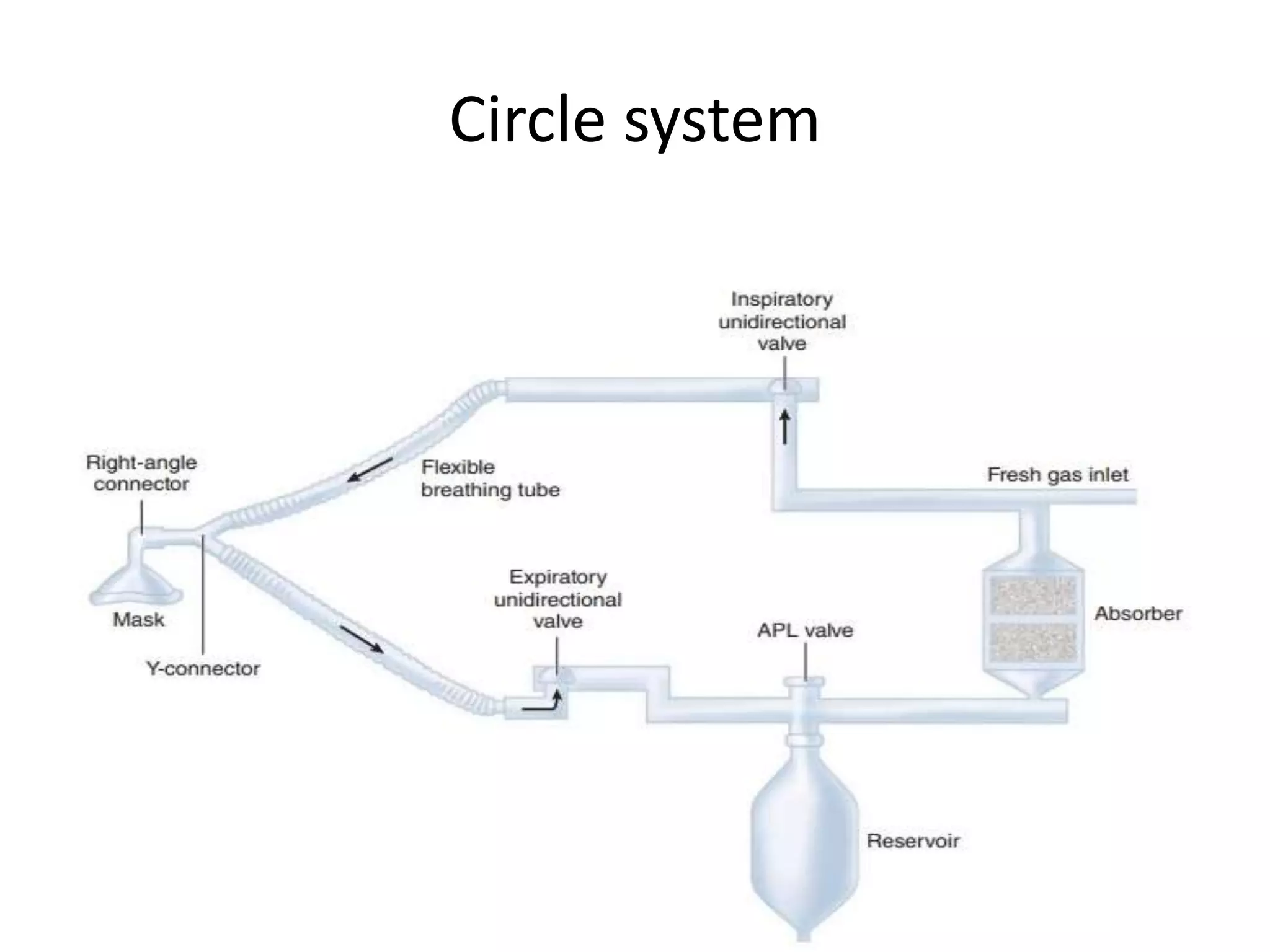
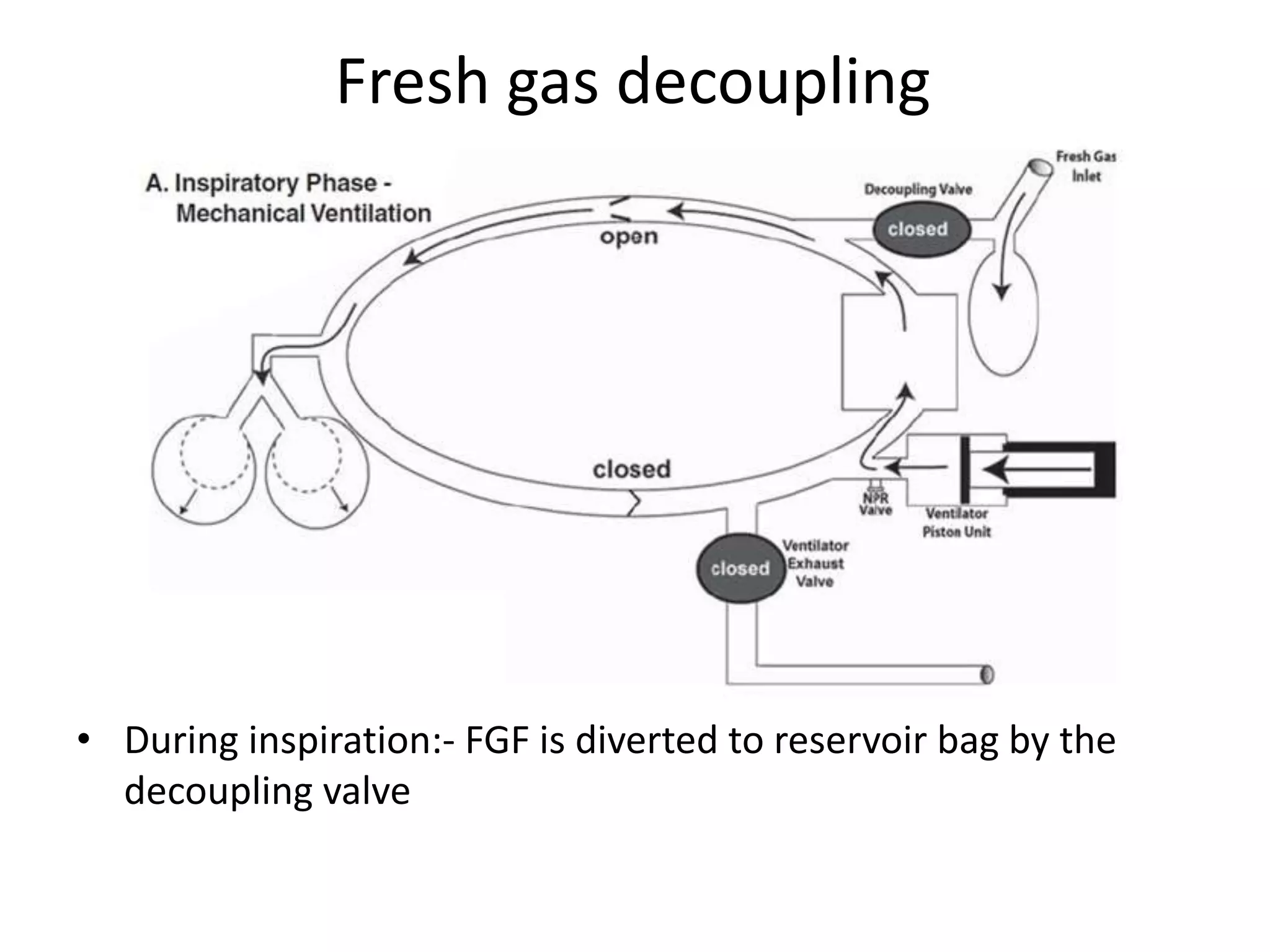
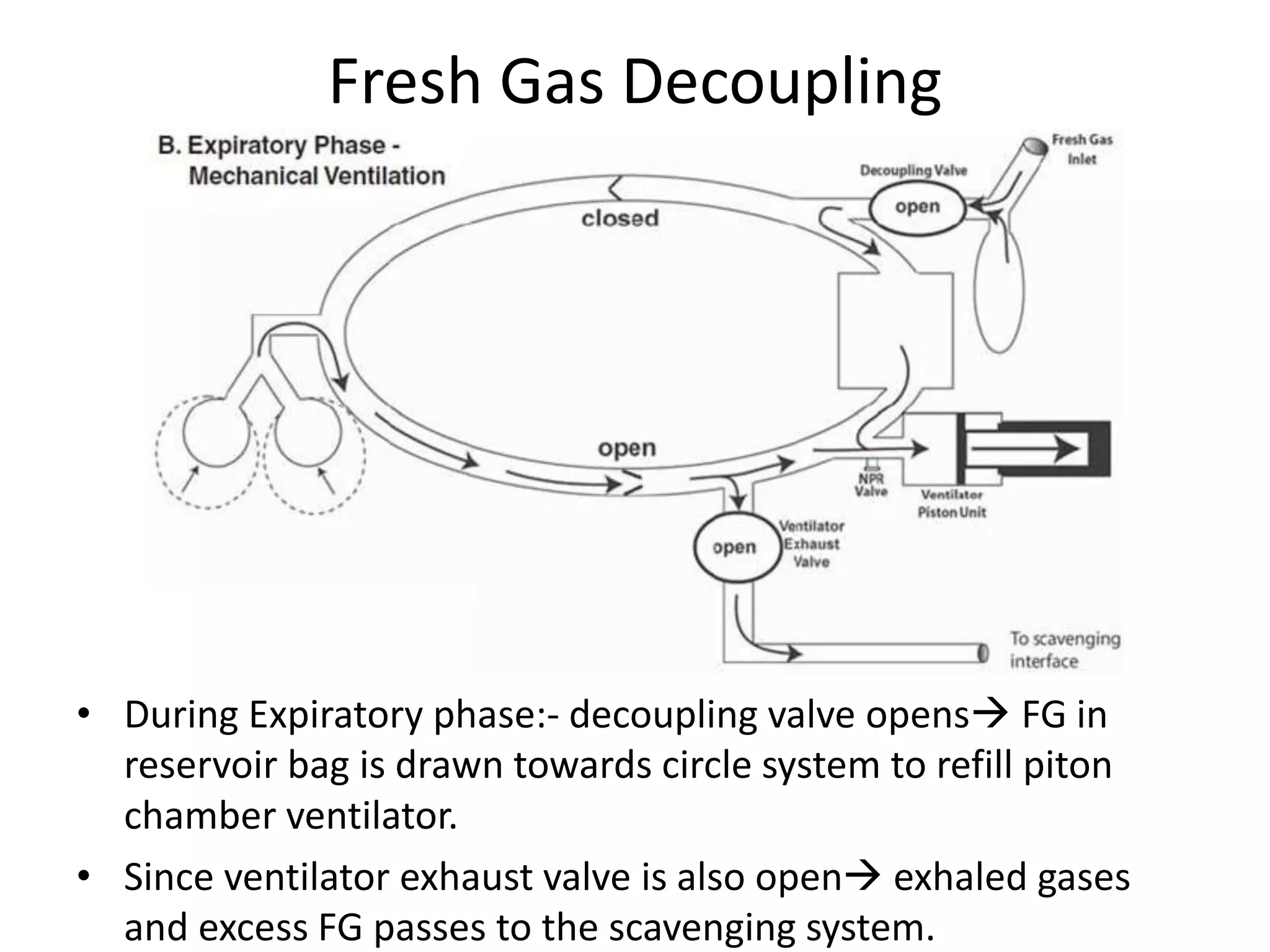
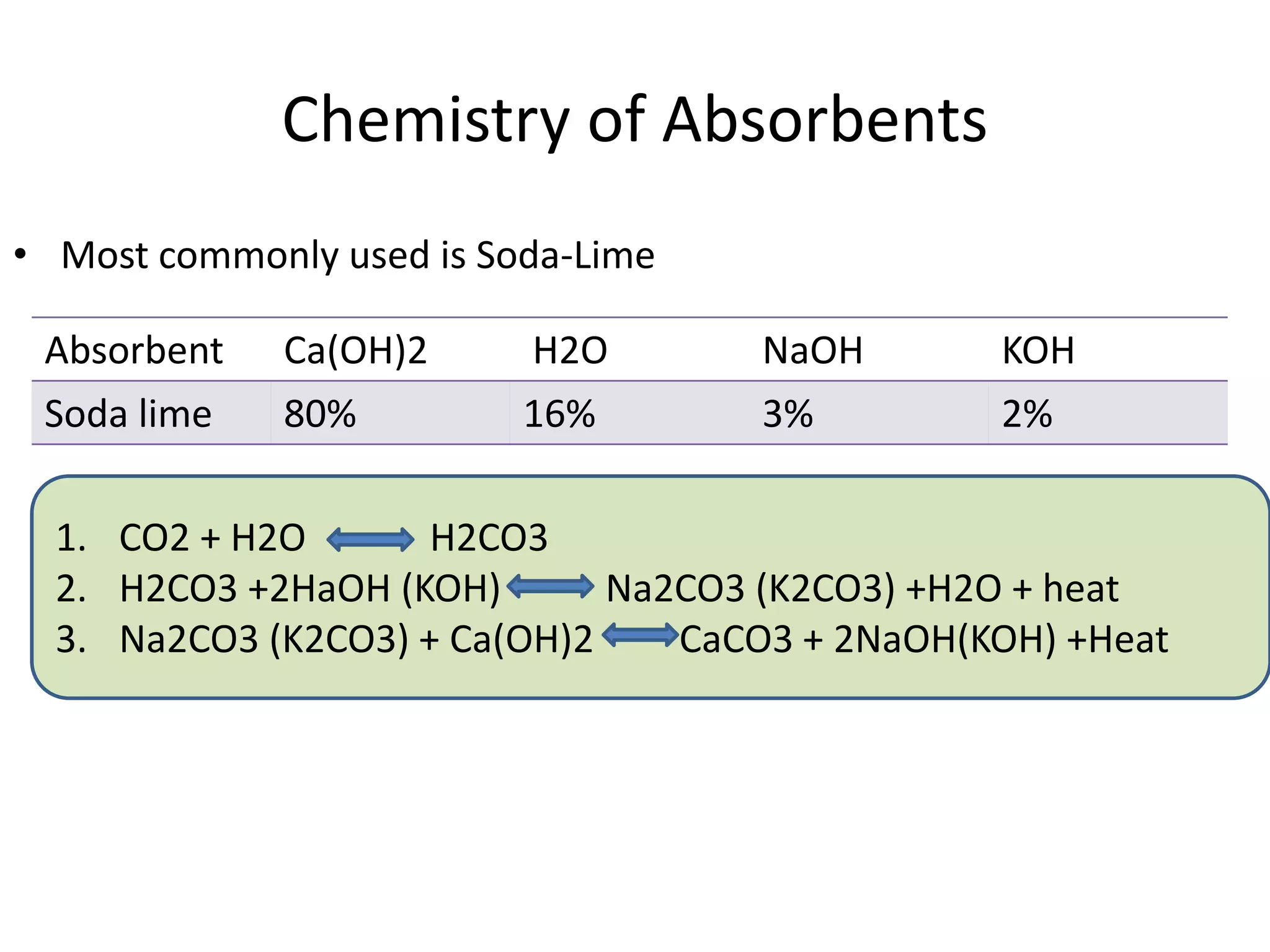
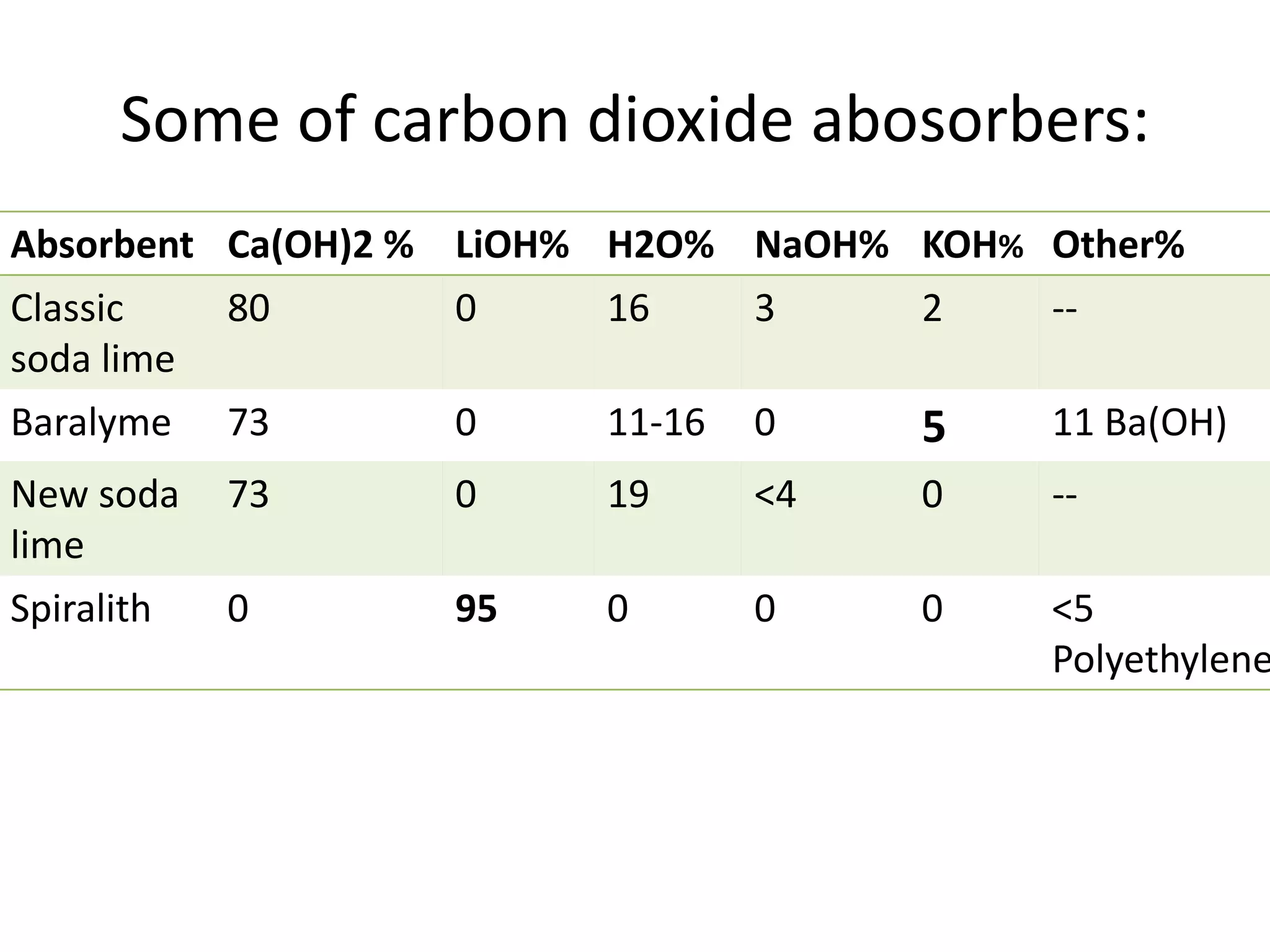
This document discusses breathing systems used during anesthesia. It begins with definitions and a brief history of breathing systems. It then classifies different breathing systems and describes the working principles and components of various systems, including Mapleson systems and the circle system. Key points covered include how fresh gas flow rates impact carbon dioxide levels, components of the circle system like the reservoir bag and carbon dioxide absorbers, and factors that influence the absorptive capacity of different carbon dioxide absorbents.