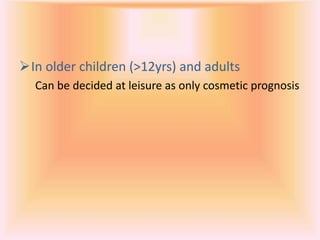
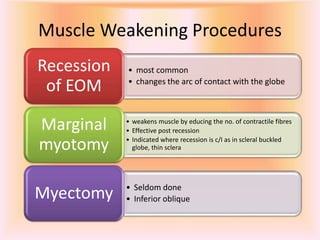
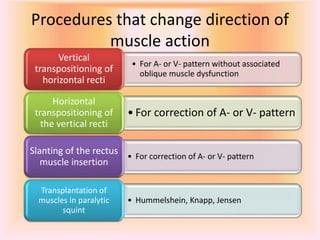
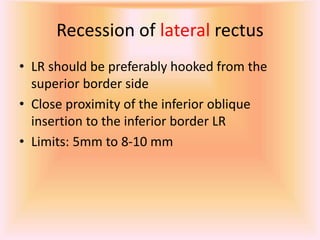
This document summarizes various squint surgeries performed by Dr. Gauree Krishnan. It discusses indications for squint surgery including correcting strabismus functionally and/or cosmetically. It describes optimal timing for surgery depending on squint type and patient age/sensory adaptations. Common surgical techniques are outlined including muscle weakening procedures like recession and marginal myotomy, and strengthening procedures like resection and advancement. General considerations for surgery and surgical steps are provided for various rectus muscle and oblique muscle procedures.