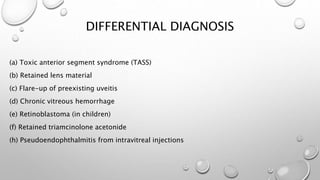
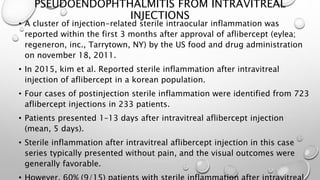
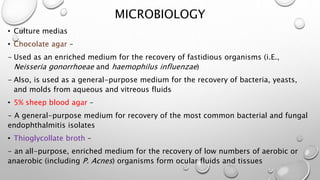
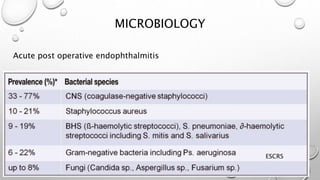
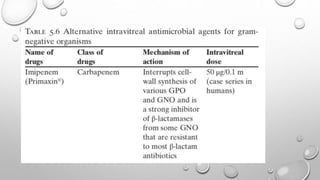
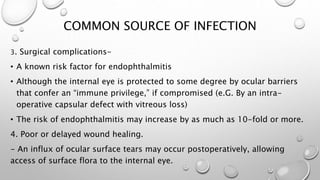
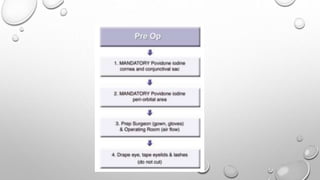
This document discusses endophthalmitis, an inflammatory condition of the eye caused by an infectious process. It defines endophthalmitis and describes the pathophysiology, including the incubation, acceleration, and destructive phases. It classifies endophthalmitis based on cause such as postoperative, post-traumatic, or endogenous. The most common causative organisms are described for each type. The diagnosis, differential diagnosis, and management including empiric antimicrobial treatment and microbiological testing are summarized.