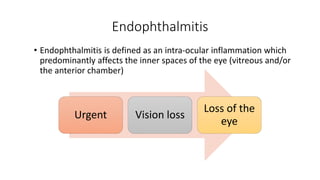
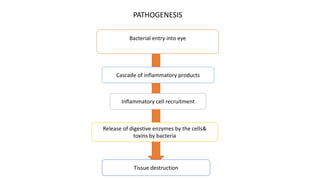
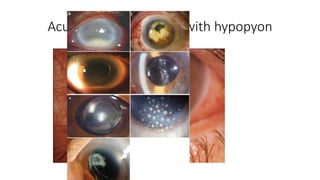
1. Endophthalmitis is an intraocular inflammation that predominantly affects the inner spaces of the eye.
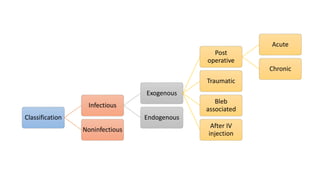
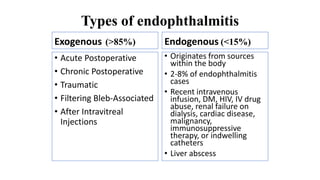
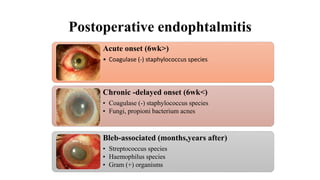
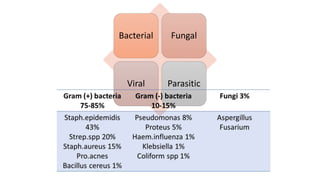
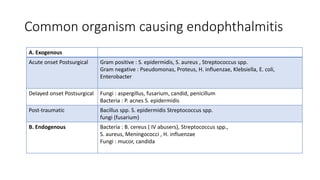
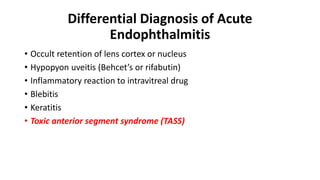
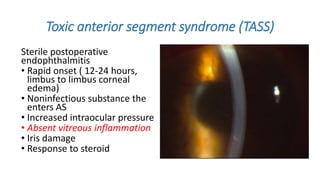
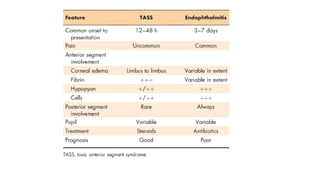
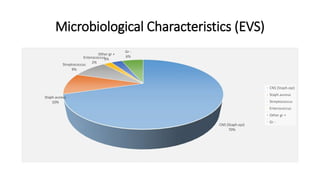
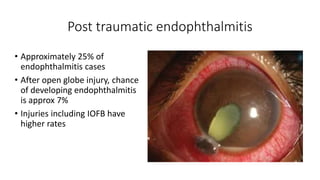
2. It can be classified as infectious (exogenous or endogenous) or non-infectious. The most common type is exogenous endophthalmitis, which accounts for over 85% of cases.
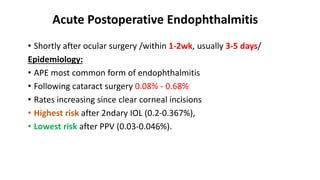
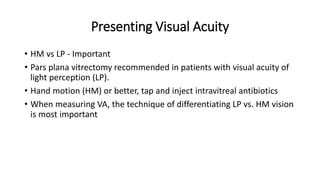
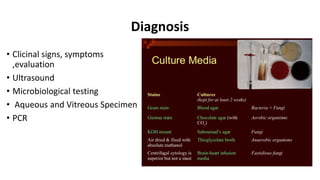
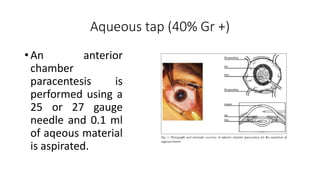
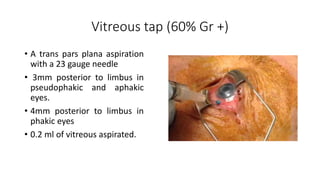
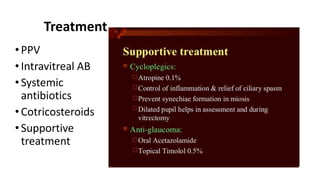
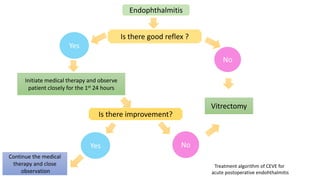
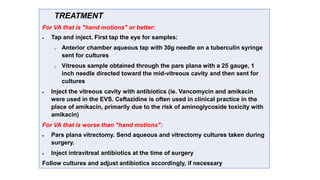
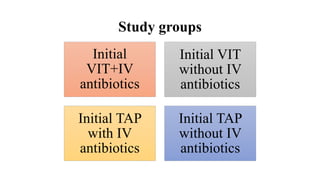
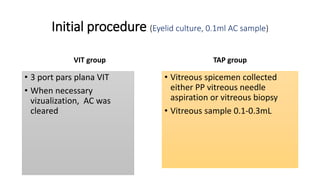
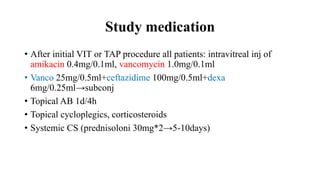
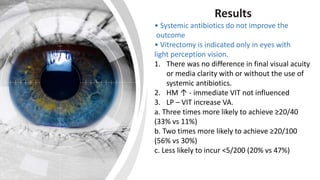
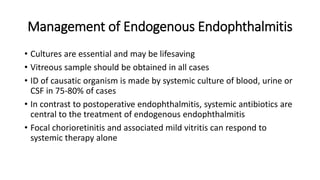
3. Treatment depends on the type and severity of endophthalmitis. For acute postoperative endophthalmitis with vision of light perception or worse, immediate pars plana vitrectomy and intravitreal antibiotics is recommended. For vision of hand motions or better, a tap and inject of intravitreal antibiotics is recommended initially.