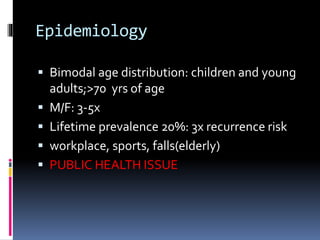
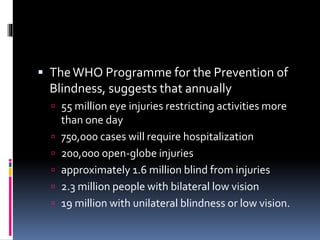
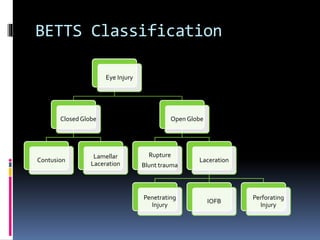
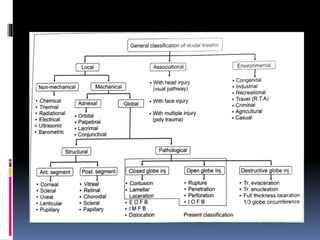
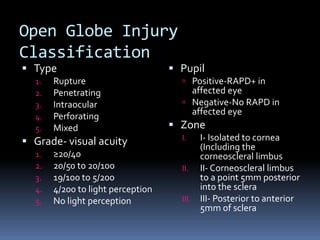
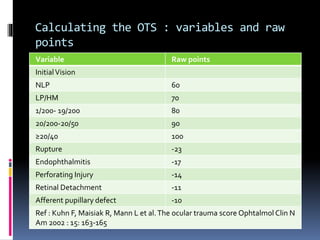
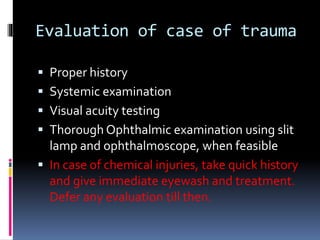
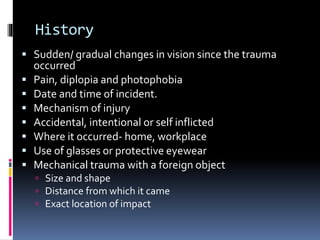
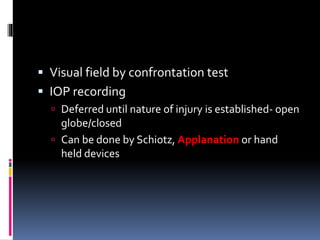
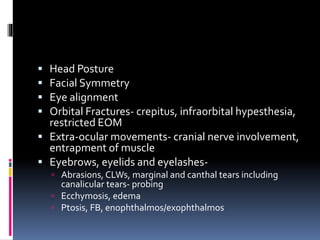
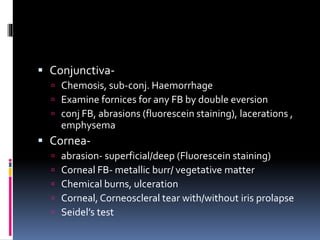
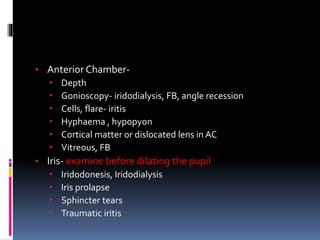
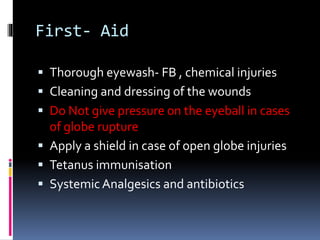
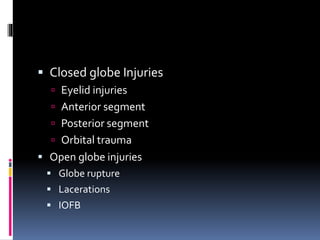
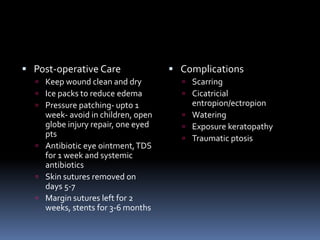
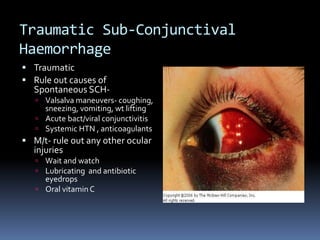
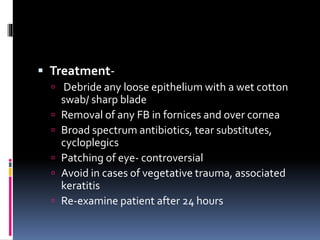
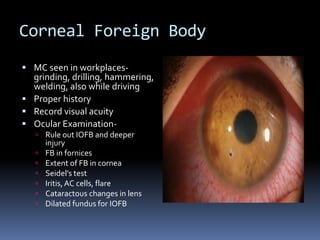
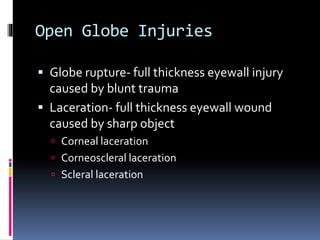
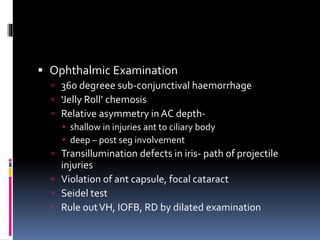
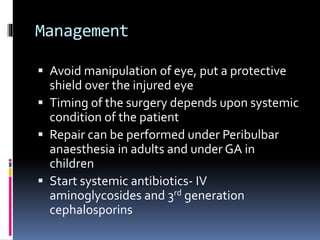
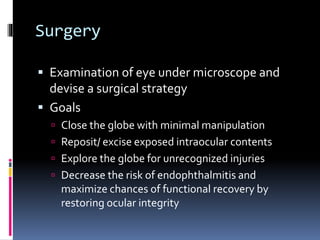
This document provides an overview of ocular trauma and basic management principles. It begins with an introduction on the importance of the eyes and prevalence of ocular trauma. It then covers epidemiology, classifications using the BETTS system, evaluation of patients, investigations, general management principles, and management of specific injuries such as closed globe, open globe, lid injuries and subconjunctival hemorrhage. The document aims to outline the evaluation and basic management of common ocular trauma presentations.















![References
Indian J Ophthalmol. 2013 Oct; 61(10):
539–540 PMCID: PMC3853447 Ocular trauma,
an evolving sub specialty Sundaram
Natarajan
Ngrel AD, Thylefors B. The global impact
of eye injuries [J] Ophthalmic Epidemiol.
1998;5:143–69. PubMed
Ocular trauma by James T. Banta
Clinical Diagnosis and management of
ocular trauma by Garg, Moreno, Shukla et
al](https://image.slidesharecdn.com/oculartrauma-150807150912-lva1-app6892/85/Ocular-trauma-108-320.jpg)