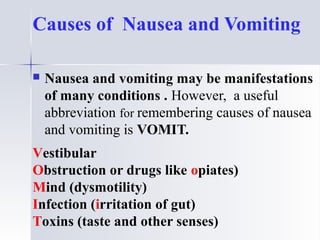
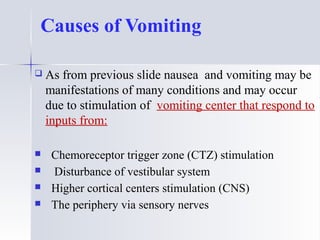
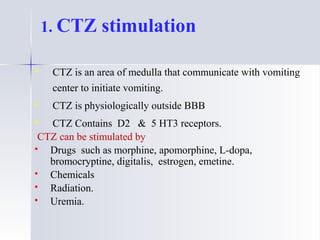
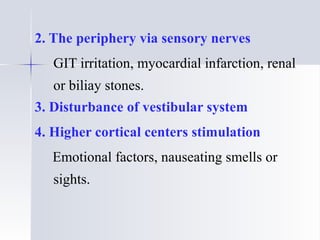
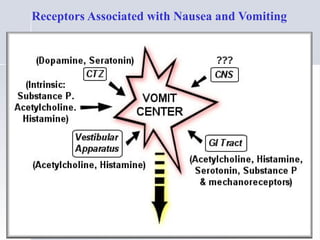
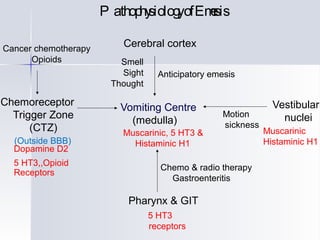
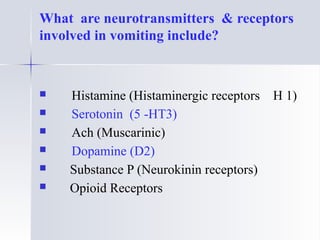
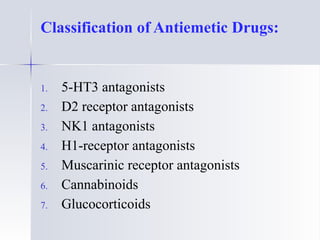
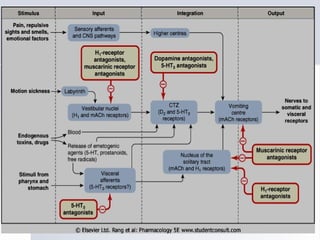
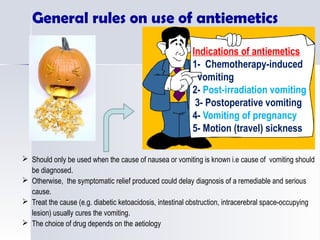
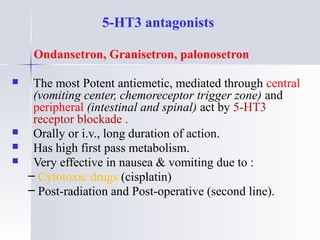
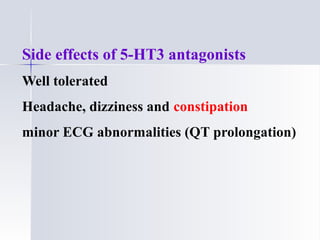
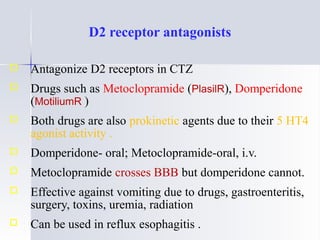
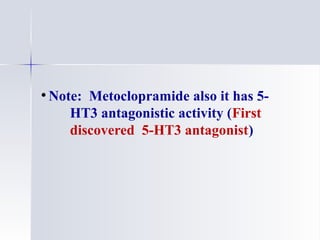
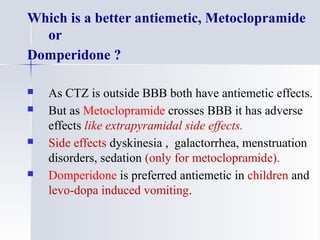
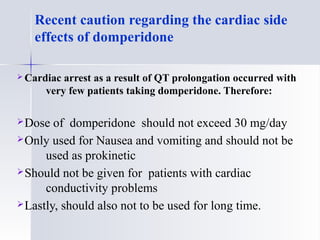
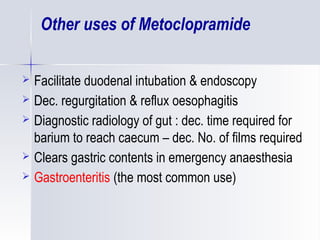
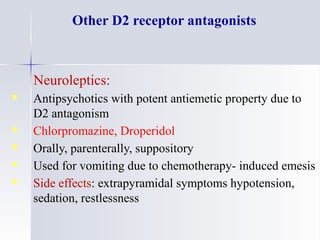
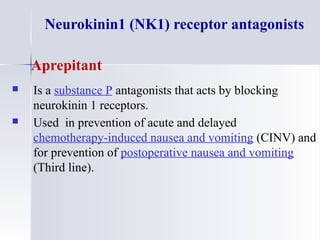
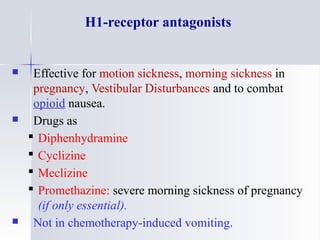
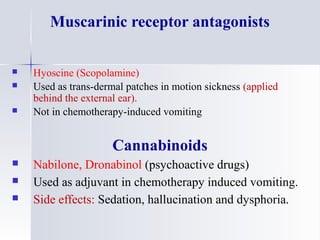
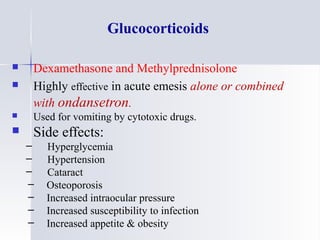
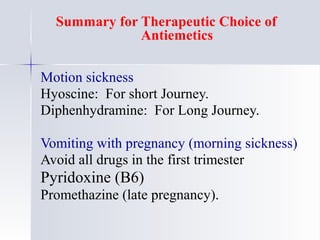
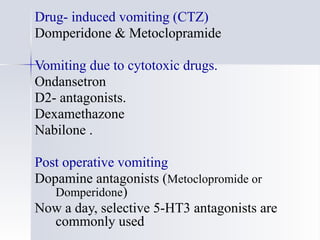
This document discusses antiemetics, which are drugs used to treat nausea and vomiting. It begins by outlining the learning objectives, which are to classify antiemetic drug classes based on mechanism of action, understand pharmacokinetics and dynamics of classes, identify drugs for specific causes, learn adjuvant antiemetics, and describe side effects. It then discusses the physiology of vomiting and consequences. Causes of nausea and vomiting are organized using the acronym VOMIT. The receptors and pathways involved are explained. The main classes of antiemetics are then described in more detail based on their receptor targets and indications. Specific drugs, dosages, advantages and side effects within each class are compared. Lastly, guidelines