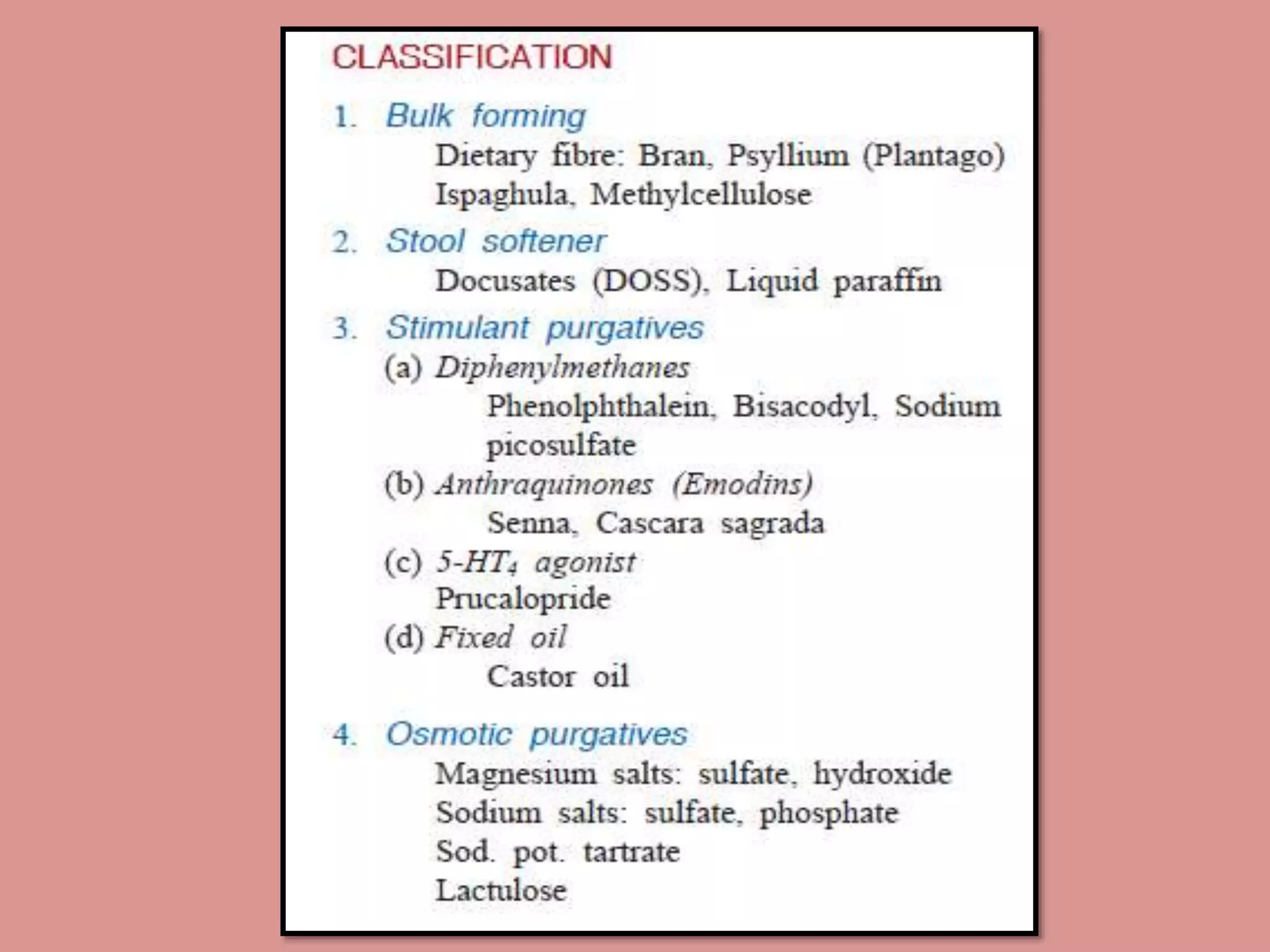
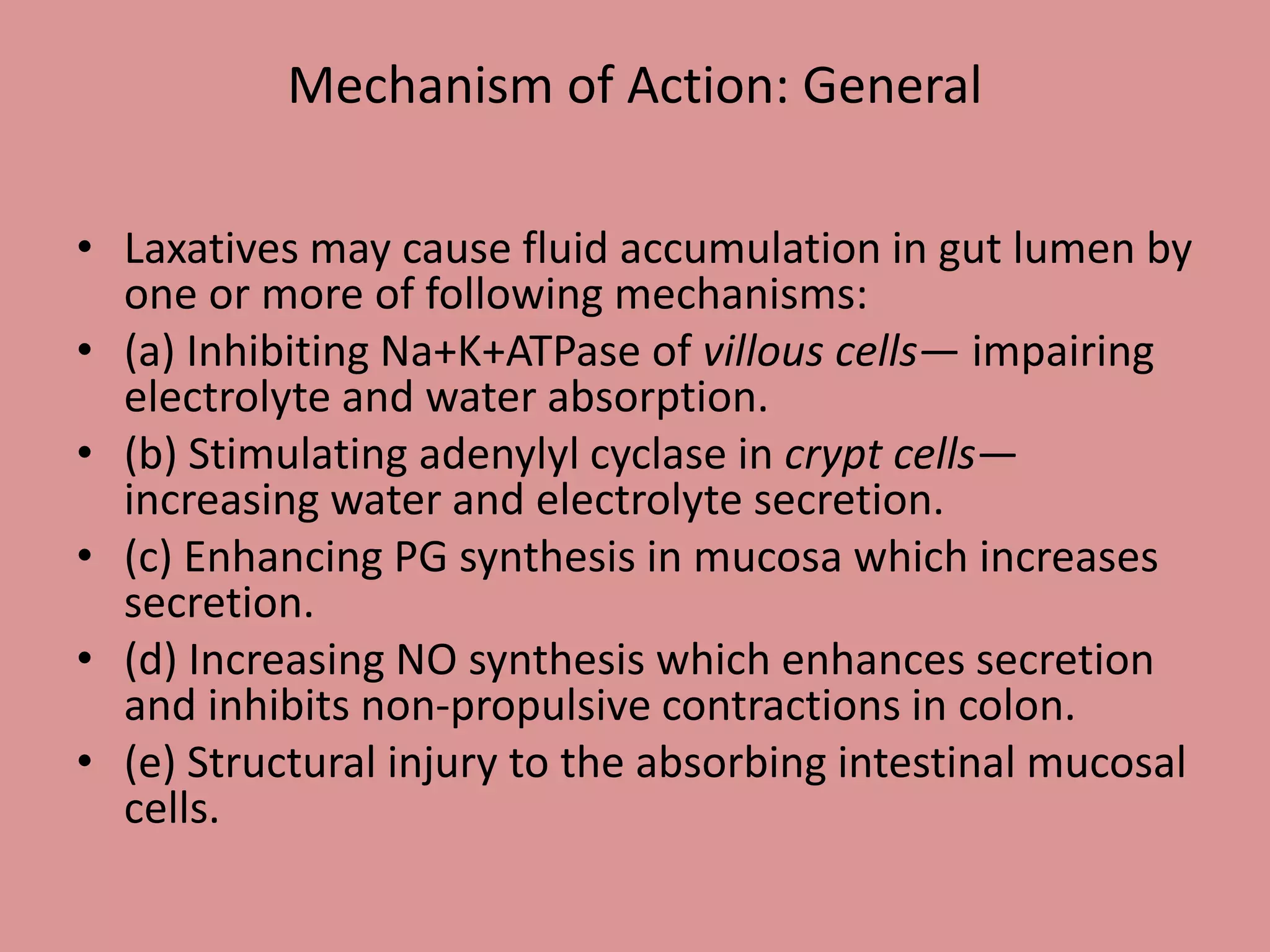
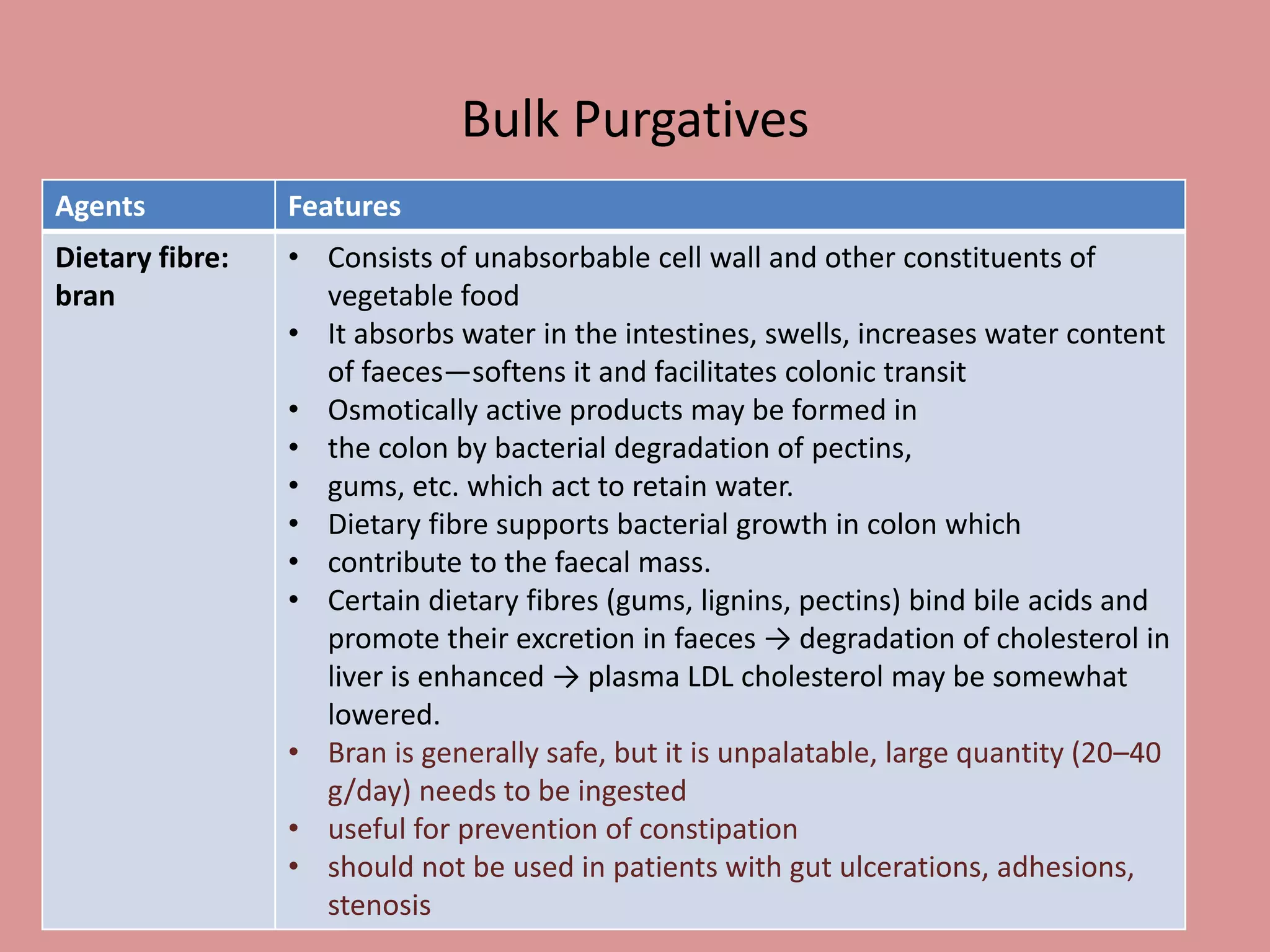
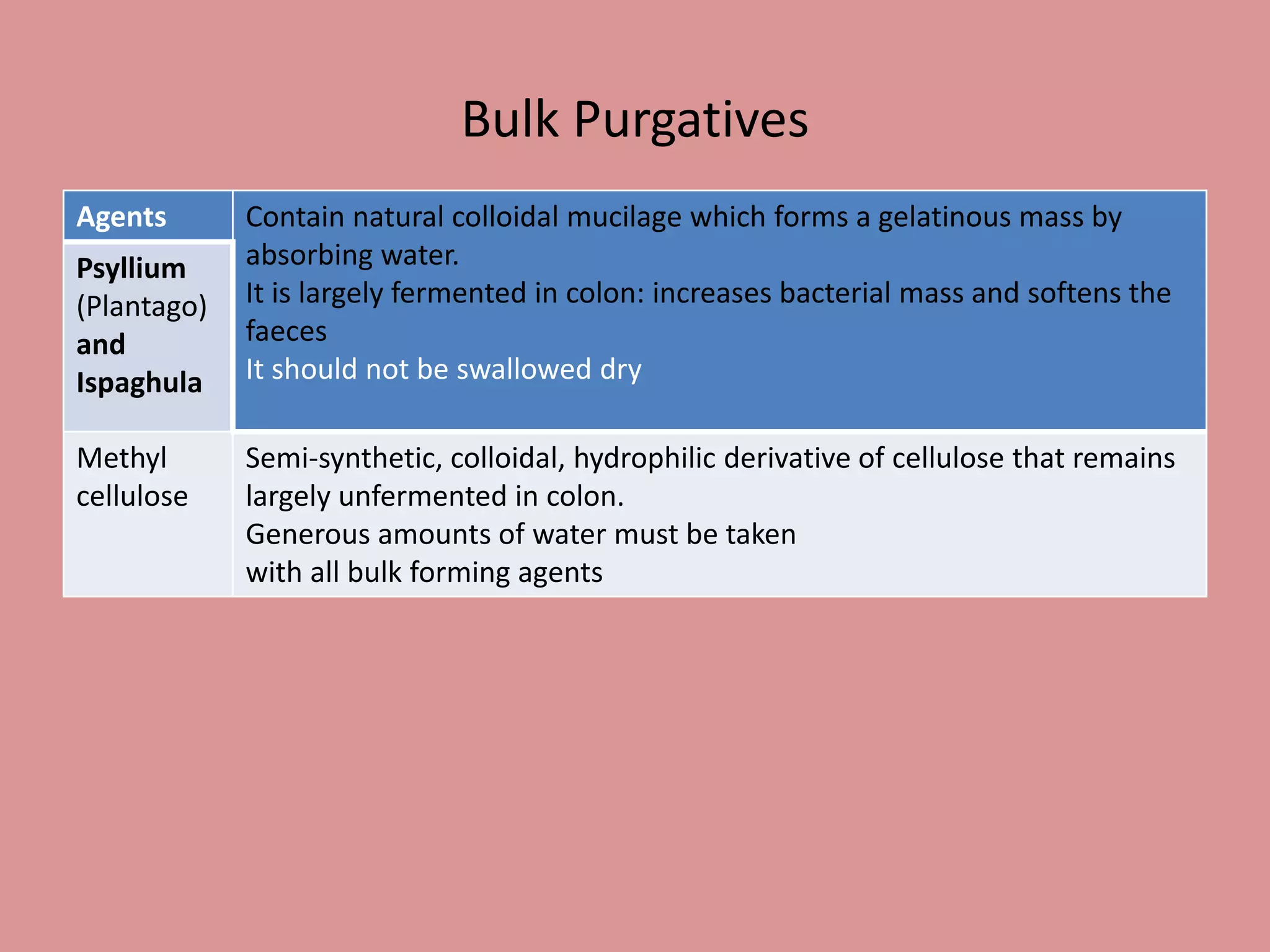
The document provides an overview of laxatives and purgatives, categorizing them into laxatives (mild action) and purgatives (stronger action), detailing their mechanisms, effects, and types, including bulk-forming agents, stool softeners, and stimulant purgatives. It discusses specific agents like dietary fiber, bisacodyl, senna, and lactulose, explaining their uses, mechanisms of action, and potential side effects. Additionally, the document outlines the applications of these medications in various clinical scenarios, such as treating constipation and preparing for medical procedures.