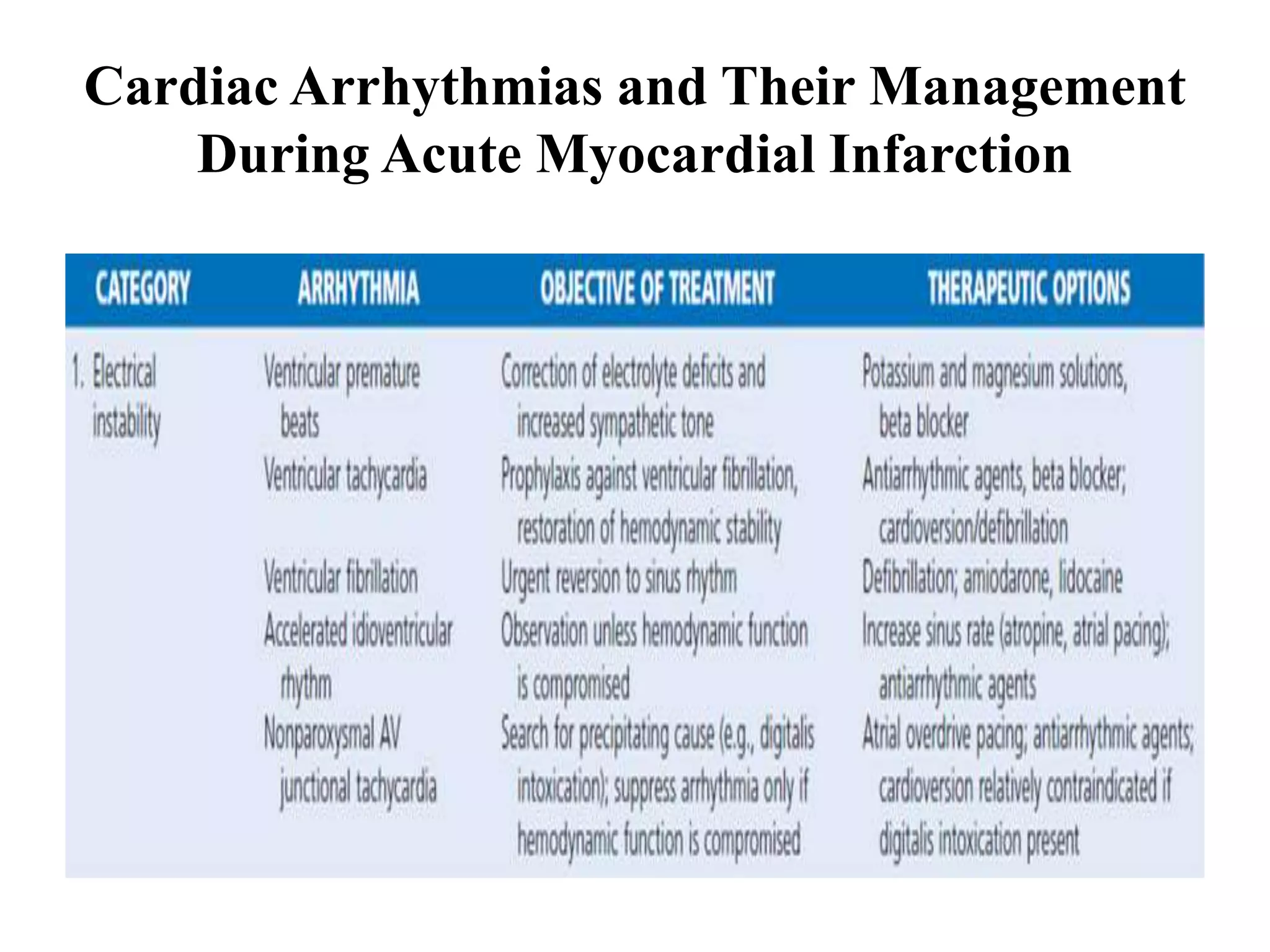
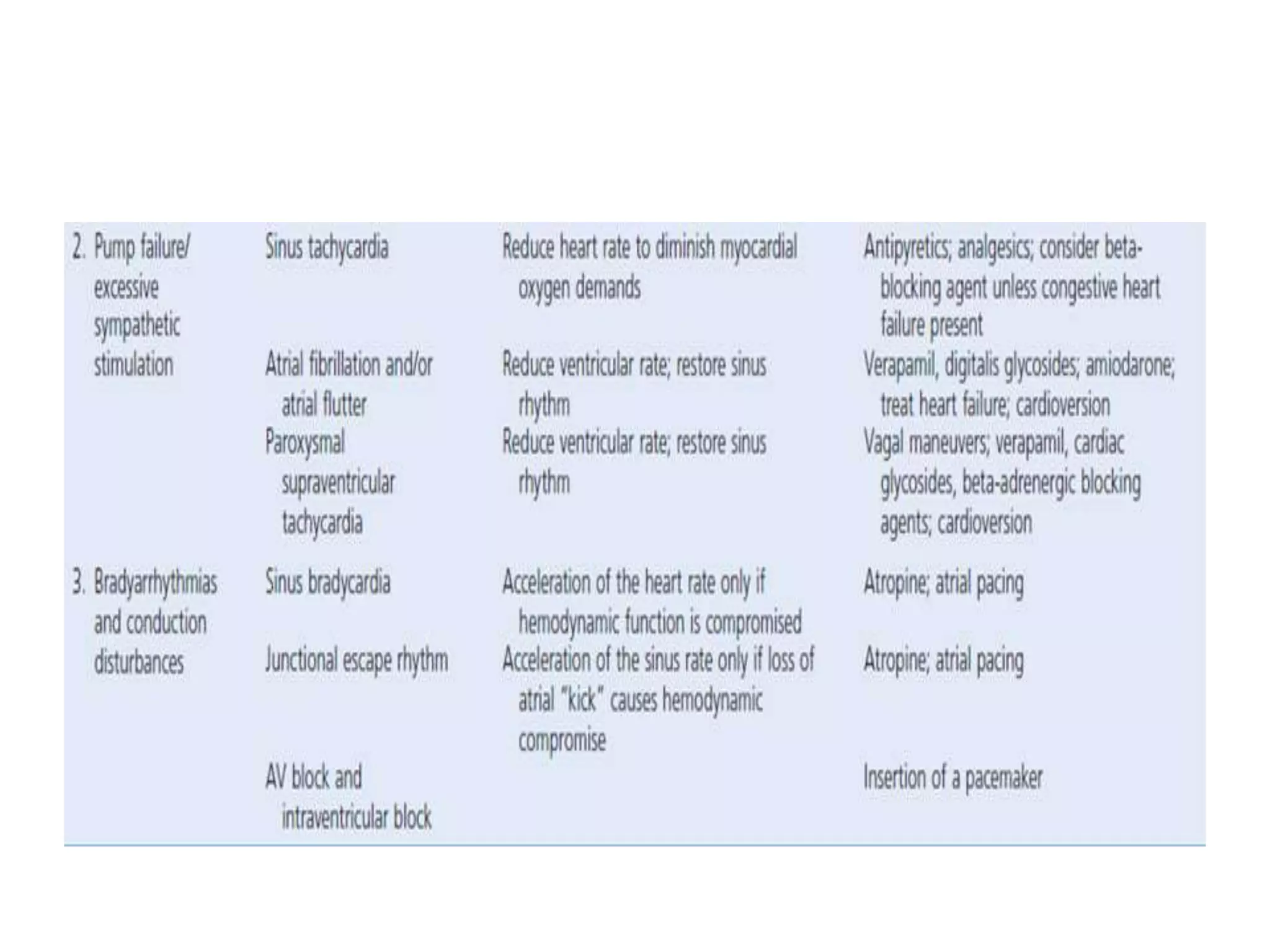
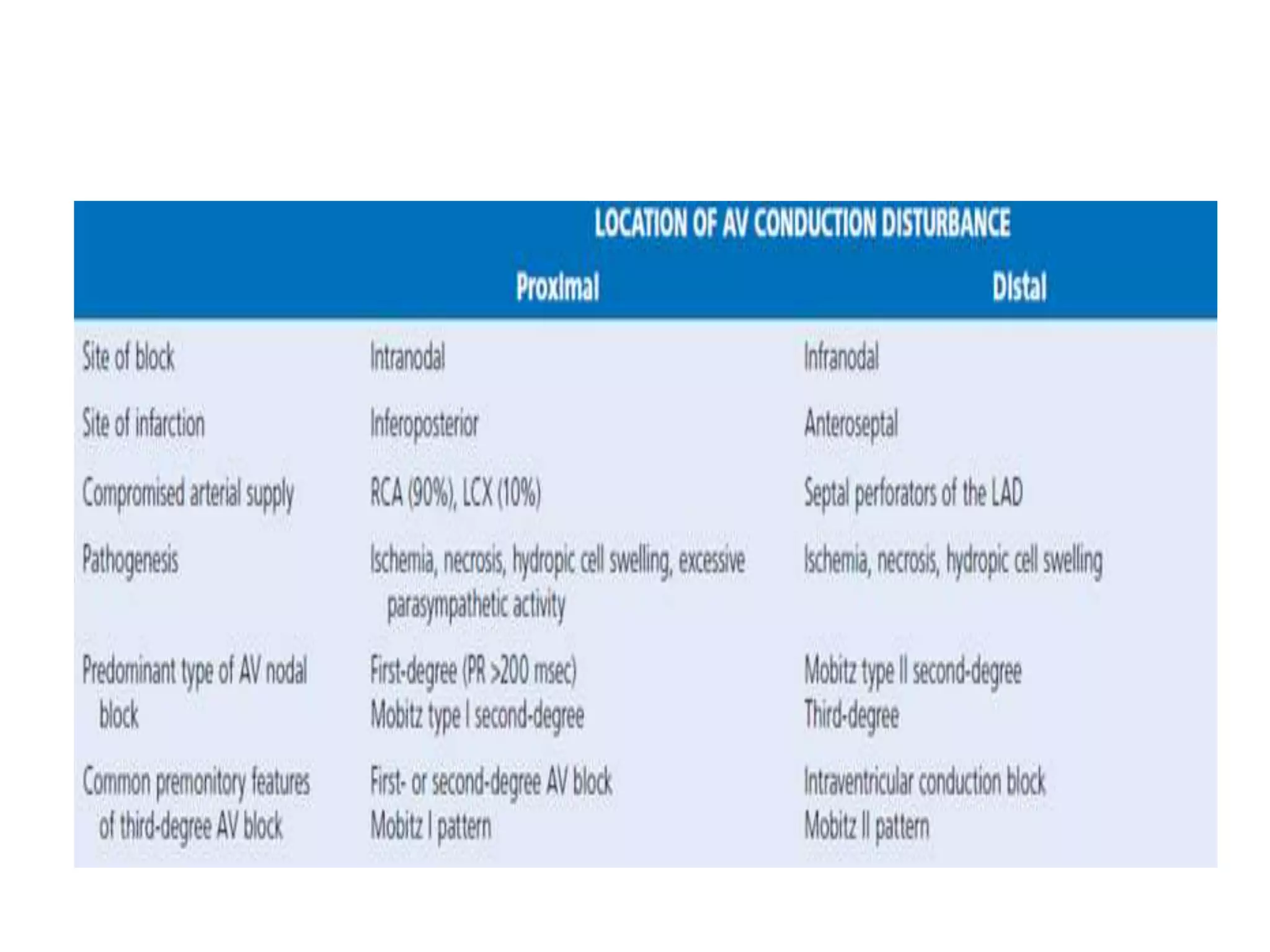
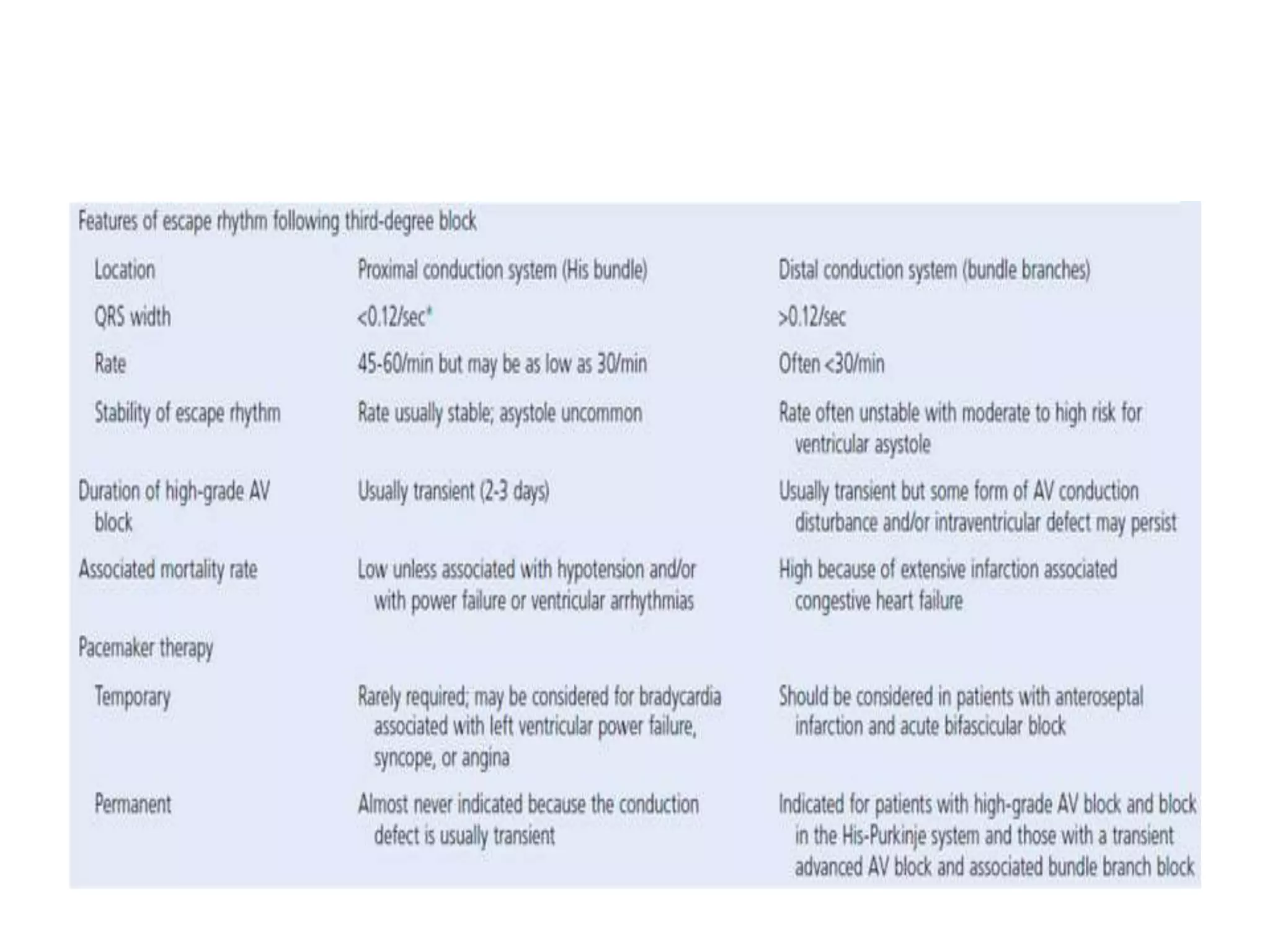
This document discusses cardiac arrhythmias and their management during acute myocardial infarction. It covers tachyarrhythmias like ventricular fibrillation and ventricular tachycardia as well as bradyarrhythmias including different types of atrioventricular block. It provides details on the mechanisms, risk factors, diagnosis and management of these arrhythmias with a focus on preventing complications through prompt treatment of underlying issues and use of drugs like beta blockers, amiodarone and pacemakers if needed.