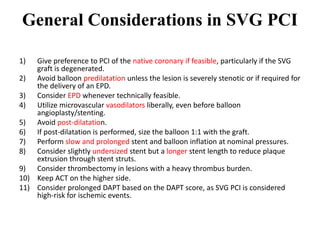
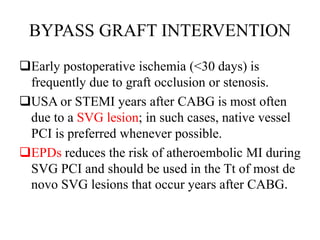
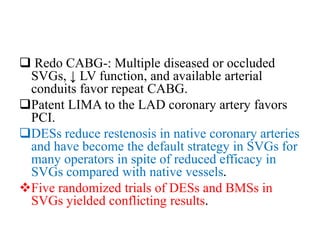
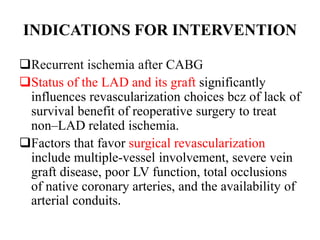
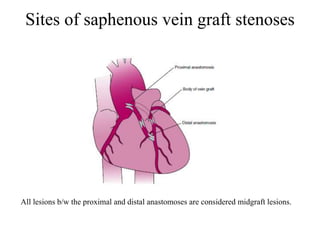
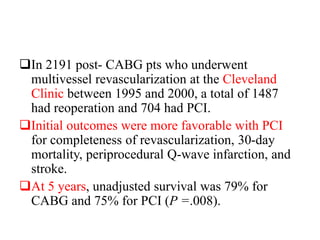
This document provides guidance on percutaneous coronary intervention (PCI) of saphenous vein grafts (SVGs). It notes that PCI of native coronary arteries is preferred when feasible. For SVG PCI, it recommends the liberal use of embolic protection devices to reduce the risk of atheroembolism. It also provides tips for technical considerations like guide catheter selection and balloon inflation pressures. It discusses the indications for and results of SVG intervention in different time periods after CABG, noting higher risks for early reintervention but short-term benefits of PCI over reoperation.
























![1. The GuardWire system (Medtronics, Minneapolis, MN
[no longer available]) .
Saphenous Vein Graft Angioplasty Free of Emboli
Randomized (SAFER) trial - 801 pt`s were randomly
assigned to stent implantation with or without use of
the GuardWire distal protection device.
This study is the only RCT of EPD vs no protection.
30day MACEs were reduced by 42% with use of EPD
(16.5% to 9.6%, P = .004), primarily bcz of the lower
rates of MI.](https://image.slidesharecdn.com/bypassgraftintervention2-210711171810/85/Bypass-graft-intervention2-41-320.jpg)