The document discusses hypotonia in infants and provides details on:
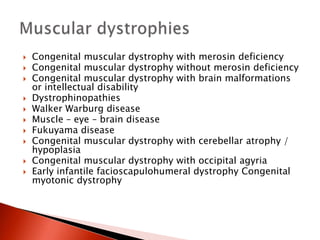
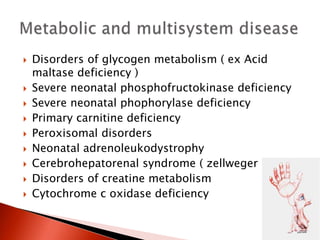
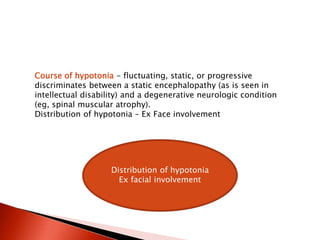
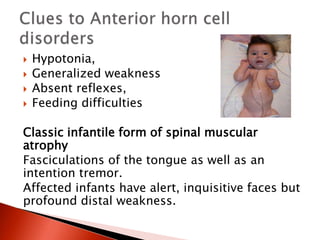
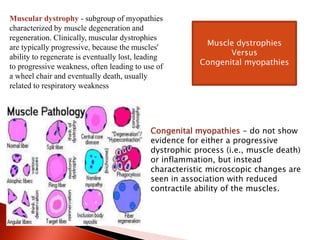
- The differential diagnosis of hypotonia includes both benign and serious conditions.
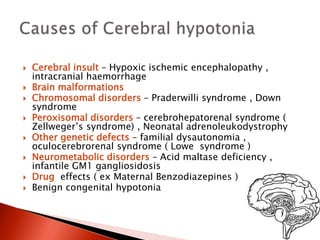
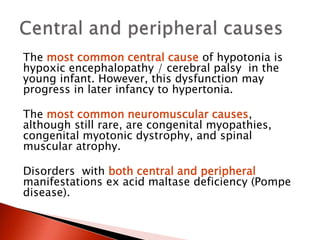
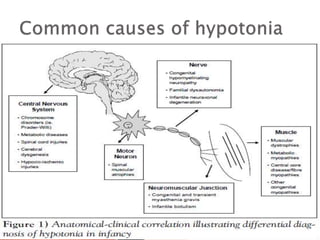
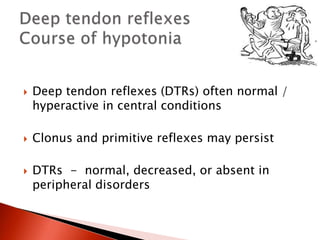
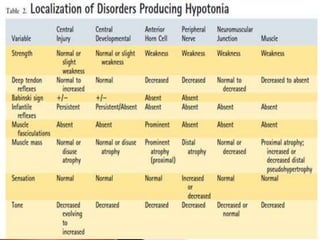
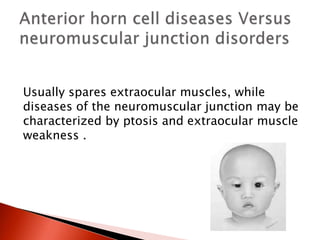
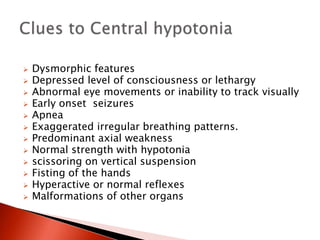
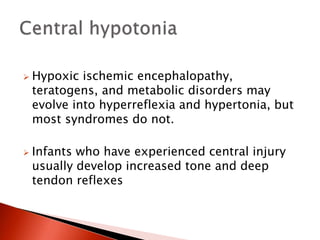
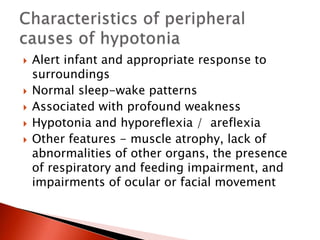
- Hypotonia can be caused by central nervous system issues or peripheral nervous system issues. Central causes account for 60-80% of cases.
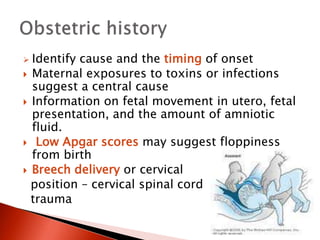
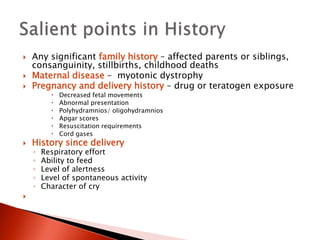
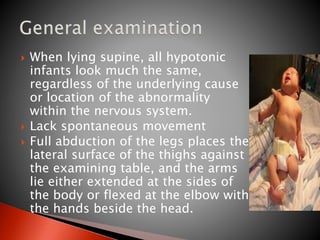
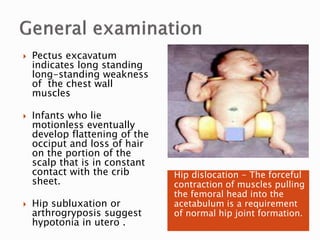
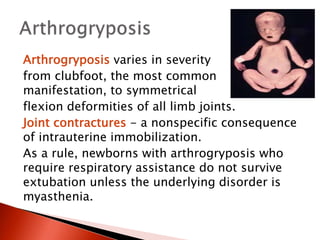
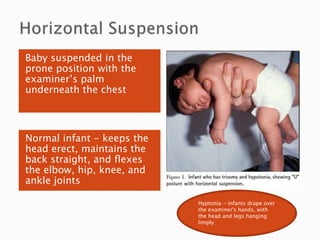
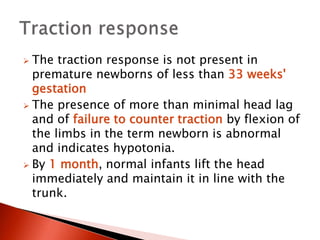
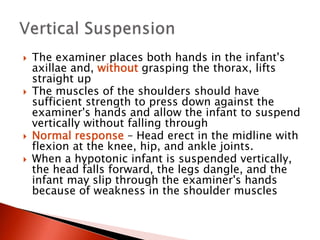
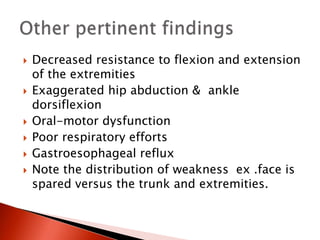
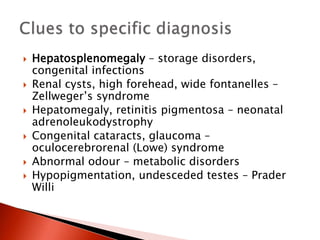
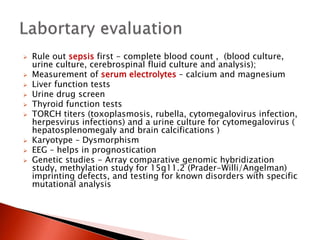
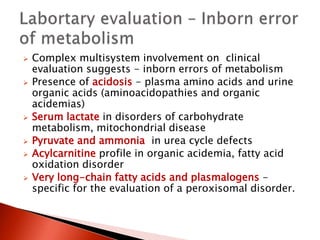
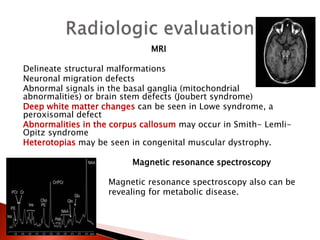
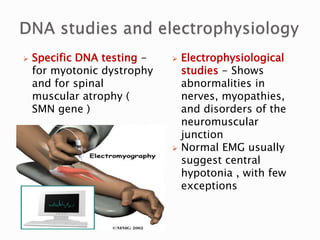
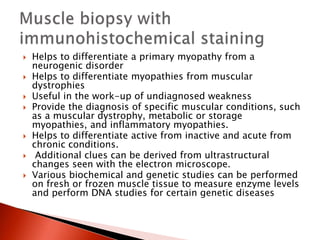
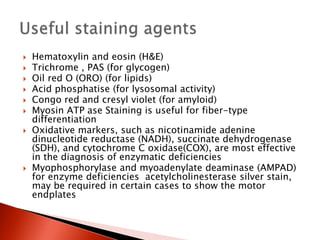
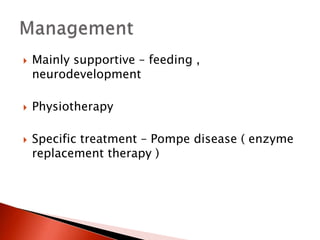
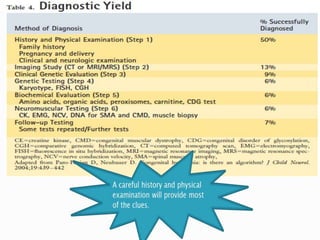
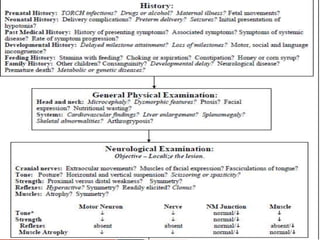
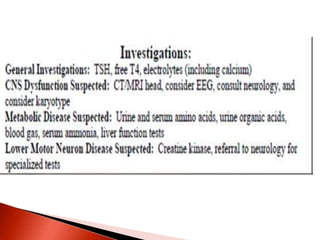
- The evaluation of an infant with hypotonia includes a detailed history, physical exam focusing on tone and strength, and initial screening tests. Further testing may include imaging, genetic testing, and metabolic testing depending on exam findings.