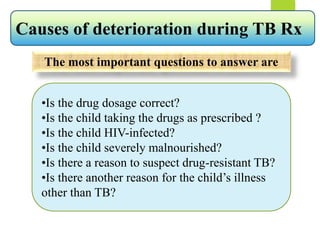
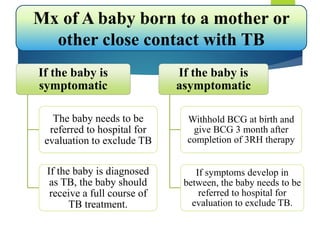
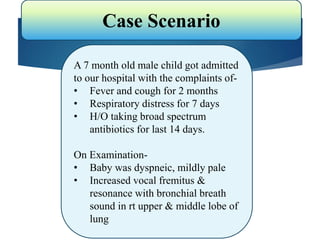
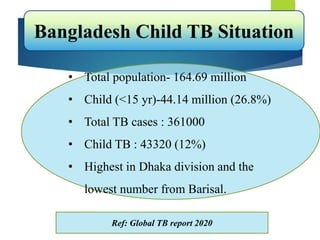
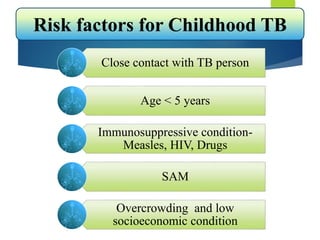
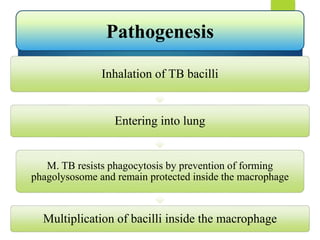
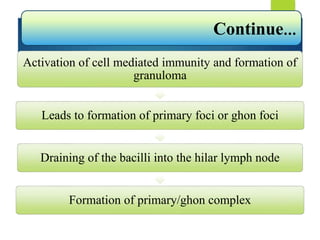
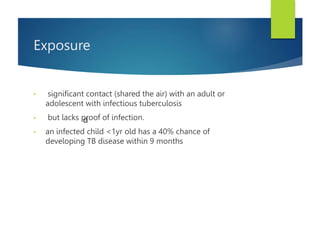
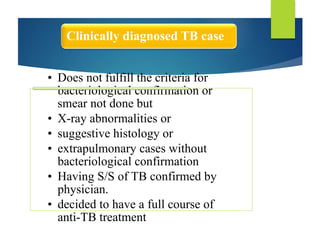
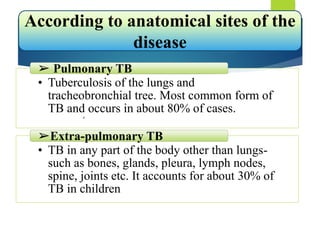
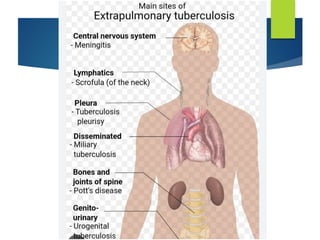
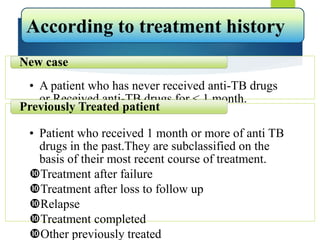
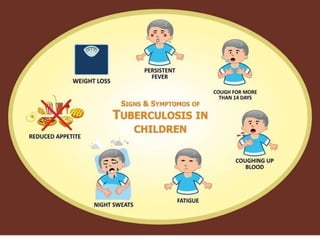
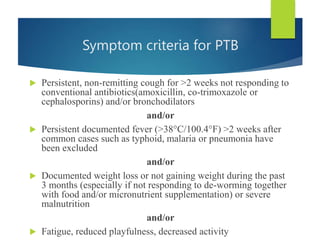
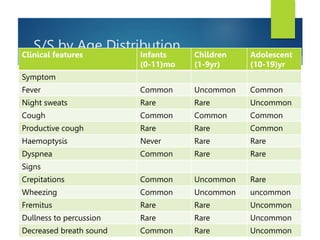
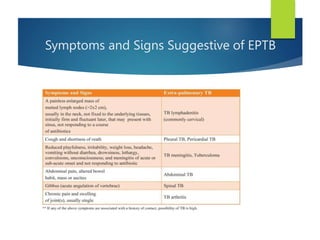
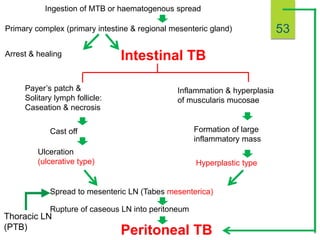
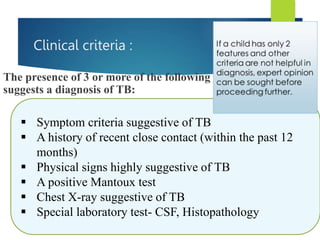
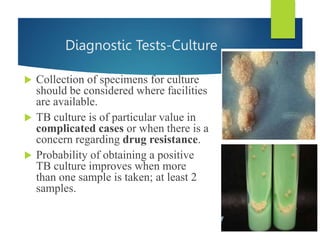
The document describes a case of a 7-month-old male child admitted to the hospital with fever and cough for 2 months, respiratory distress for 7 days, and a history of taking broad-spectrum antibiotics for 14 days. On examination, the baby was dyspneic and mildly pale with increased vocal fremitus and resonance in the right upper and middle lobe of the lung. The presentation and examination are consistent with a diagnosis of tuberculosis based on clinical criteria and history of exposure. A full course of anti-tuberculosis treatment is recommended.









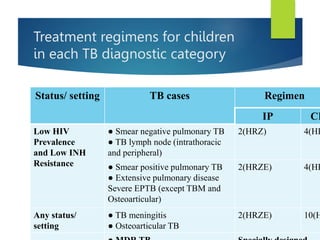
![Recommended daily dosages of
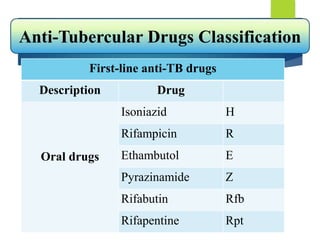
1st line anti-TB drugs
Drug Daily dose and range (mg/kg
body weight)
Isoniazid (H) 10 (07-15) [maximum 300mg]
Rifampicin (R) 15 (10-20) [maximum 600mg]
Pyrazinamide (Z) 35 (30-40) [maximum 2000mg]
Ethambutol (E) 20 (15-25) [maximum 1200mg]
Regular weight-based dose adjustment is
important, particularly in young and/or
malnourished atleast after 1, 2, 3 months
consequitively (or at a lesser interval when
necessary) and at 6 month .](https://image.slidesharecdn.com/seminar-1-230917114810-d407756a/85/Seminar-1-pptx-100-320.jpg)