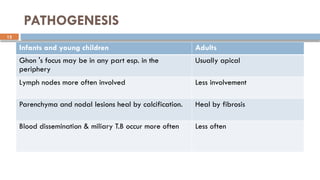
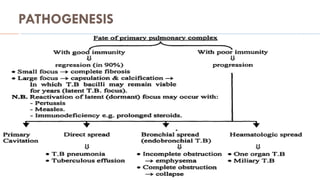
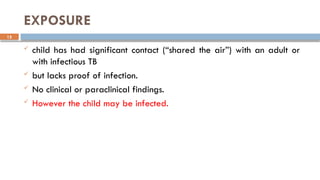
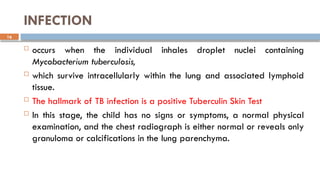
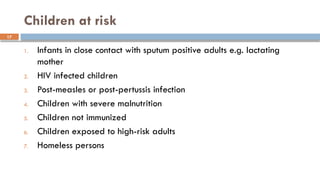
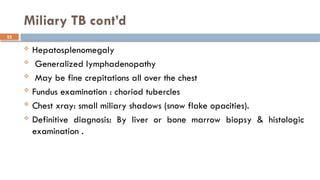
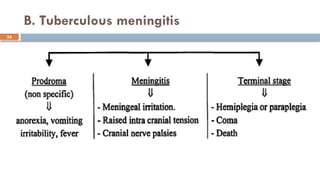
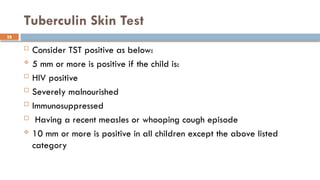
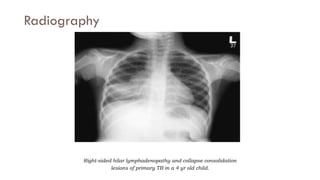
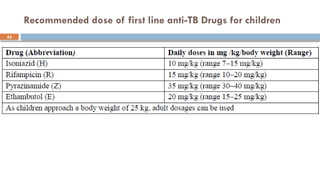
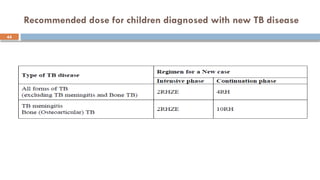
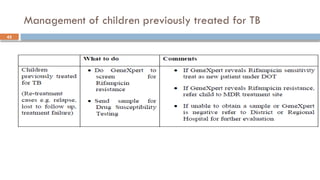
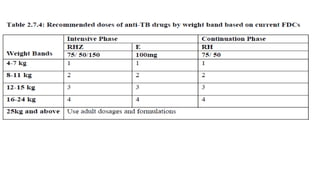
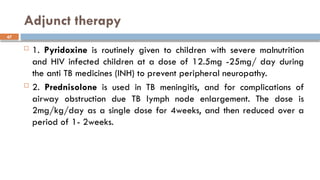
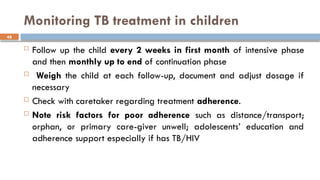
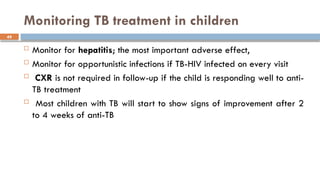
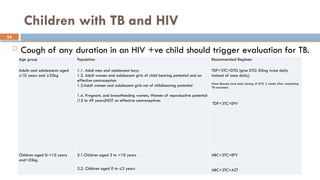
The document is a comprehensive overview of tuberculosis (TB) in children, covering its introduction, etiology, pathogenesis, clinical presentation, diagnosis, treatment, and prevention strategies. It highlights the epidemiology of childhood TB, transmission modes, and risk factors for infection and disease progression, while detailing the importance of early detection and management. The management section emphasizes the need for effective treatment, monitoring, and prevention techniques such as BCG vaccination and isoniazid preventive therapy (IPT) for at-risk populations.