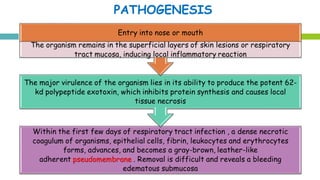
This document discusses diphtheria, an infectious disease caused by the bacteria Corynebacterium diphtheriae. It produces an exotoxin that can cause local infection in the throat and airways and lead to complications affecting the heart, kidneys and nerves if the toxin spreads systemically. Clinical manifestations depend on the site of infection and may include pseudomembrane formation. Diagnosis involves culture, microscopy and toxin testing. Treatment is with antitoxin to neutralize the toxin as well as antibiotics. Active immunization with diphtheria, tetanus and pertussis vaccine (DwPT or TdaP) provides protection.