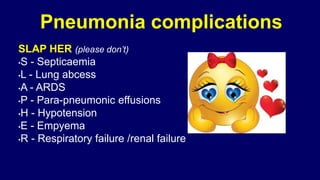
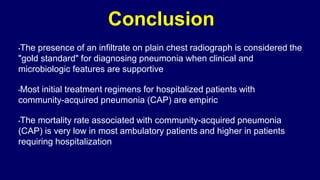
The document is a detailed examination of pneumonia, including its diagnosis, management, and complications. It outlines various classifications, risk factors, clinical features, investigations, treatment strategies, and preventive measures associated with pneumonia. It also emphasizes the importance of empirical treatment in hospitalized patients and highlights the significant variability in outcomes based on patient condition.















































![Outpatients Treatment(empirical)
Previously healthy and no antibiotics in past 3 months
•A macrolide (clarithromycin or azithromycin or
Doxycycline )
Comorbidities or antibiotics in past 3 months:
•Respiratory fluoroquinolone [moxifloxacin ,levofloxacin ] or β-
lactam ( high-dose amoxicillin or amoxicillin/clavulanate)](https://image.slidesharecdn.com/pneumoniaaslam-160429093234/85/Pneumonia-54-320.jpg)
![Inpatients, non-ICU
•A respiratory fluoroquinolone [moxifloxacin ,levofloxacin ]
•β -lactam [cefotaxime ,ceftriaxone ,ampicillin] plus a
macrolide [oral clarithromycin or azithromycin)](https://image.slidesharecdn.com/pneumoniaaslam-160429093234/85/Pneumonia-55-320.jpg)