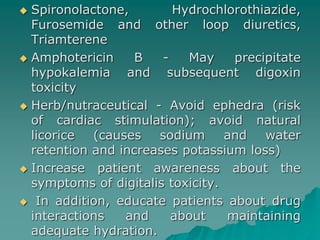
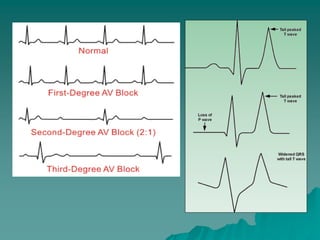
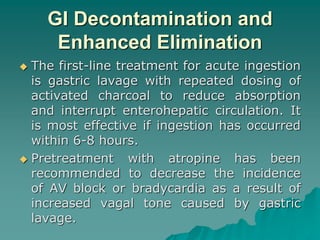
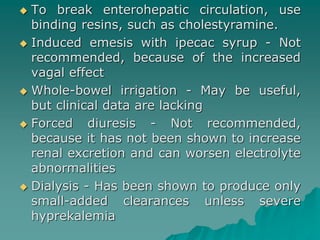
Digoxin toxicity is caused by digoxin, a plant-derived cardiac glycoside used to treat heart conditions. It has a narrow therapeutic window, so toxicity can easily occur. Common signs of toxicity include arrhythmias such as heart block or tachycardia. Management involves discontinuing digoxin, treating arrhythmias, correcting electrolyte imbalances, and using digoxin antibody fragments for severe toxicity. Factors like renal impairment, hypokalemia, and drug interactions can precipitate or worsen digoxin toxicity.


![ Cardiac fiber [Ca2+] is exchanged for
extracellular sodium (3:1 ratio) by by
Na+/Ca+ exchanger transport system that
is driven by the concentration gradient for
these ions and the transmembrane
potential; increase in [Na+]i is related
crucially to the positive inotropic effect of
digitalis.
Facilitation of Ca+ entry through the
voltage gated Ca+ channels of the
membrane. That is associated with
increase in slow inward calcium current
during the plateau of action potential.](https://image.slidesharecdn.com/digoxintoxicity-141014042316-conversion-gate02/85/Digoxin-toxicity-4-320.jpg)