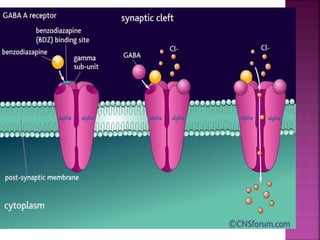
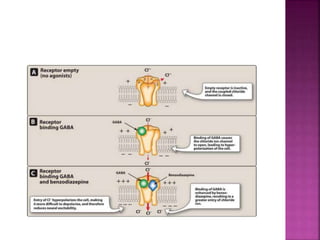
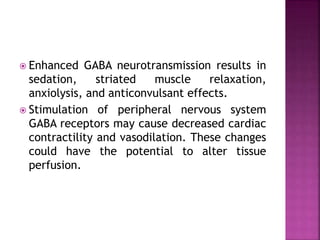
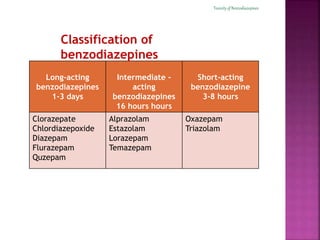
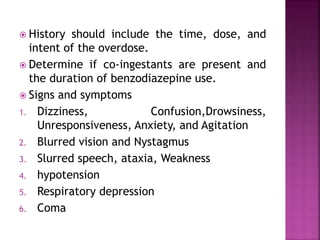
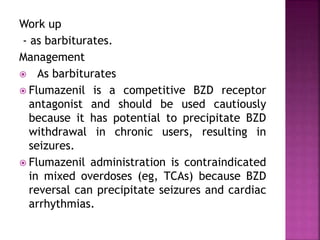
Benzodiazepines are commonly prescribed sedative-hypnotic agents that were introduced in 1960. They are used for conditions like anxiety, insomnia, alcohol withdrawal, and seizures by enhancing the effects of the inhibitory neurotransmitter GABA. While generally safe, benzodiazepines can cause side effects with prolonged use or overdose like dependence, withdrawal symptoms, and respiratory depression. The effects of different benzodiazepines vary based on their ability to cross the blood-brain barrier and metabolism, with short-acting agents having faster onsets but shorter durations of action.