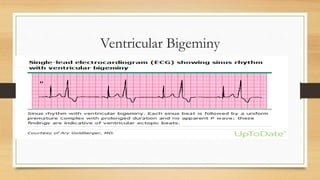
Digoxin toxicity can cause various arrhythmias due to its effects on intracellular calcium levels and vagal tone. Life-threatening arrhythmias may occur at plasma digoxin levels above 2.0 ng/mL. Hypokalemia and age over 65 increase toxicity risk. Symptoms include ectopic atrial tachycardia with block, various forms of AV block, and junctional rhythms. Distinguishing features between arrhythmias is important for appropriate treatment.




![• Retrospective analysis of data from the large digitalis investigation group
(DIG trial) revealed that serum digoxin levels ranging from 1.2 to 2.0 ng/mL
(1.5 to 2.6 nmol/L) were associated with an excess mortality versus placebo
in women with heart failure .
• Therefore, we recommend maintaining trough digoxin levels at the lower
range (eg, between 0.5 and 0.8 ng/mL [0.6 to 1.0 nmol/L]) in both male and
female patients to help minimize toxicity](https://image.slidesharecdn.com/digoxintoxicity-210719083507/85/Digoxin-toxicity-8-320.jpg)