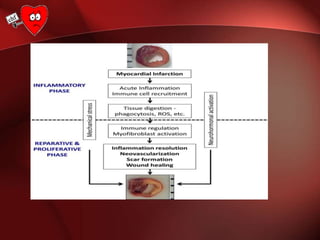
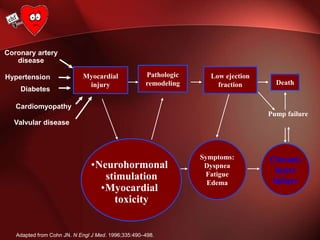
The document discusses the biological basis of cardiac repair after myocardial infarction. It notes that massive cardiomyocyte loss due to infarction overwhelms the heart's limited regenerative capacity, resulting in scar formation. Necrotic cells trigger an intense inflammatory response through danger signals and toll-like receptor signaling that recruits leukocytes. As inflammation subsides, fibroblasts proliferate and deposit collagen, maintaining ventricular integrity. Dysregulated inflammation, impaired resolution, or excessive fibrosis can cause adverse remodeling and heart failure. Modulating the inflammatory and reparative response may prevent post-infarction heart failure.




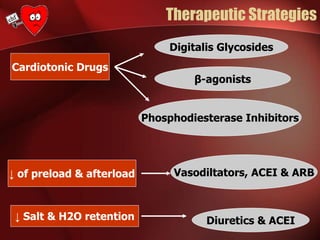
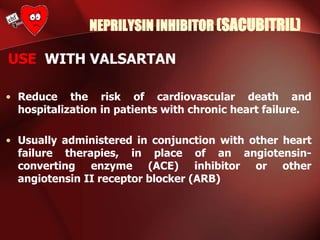
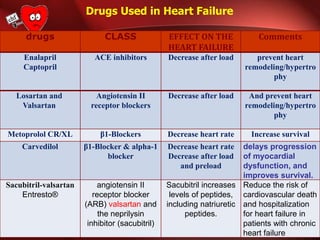
![NEPRILYSIN INHIBITOR (SACUBITRIL)
Mechanism of Action
Prodrug that inhibits neprilysin (neutral endopeptidase
[NEP]) through the active metabolite LBQ657, leading
to increased levels of peptides, including natriuretic
peptides.](https://image.slidesharecdn.com/heartfailure-211205224700/85/Heart-failure-30-320.jpg)