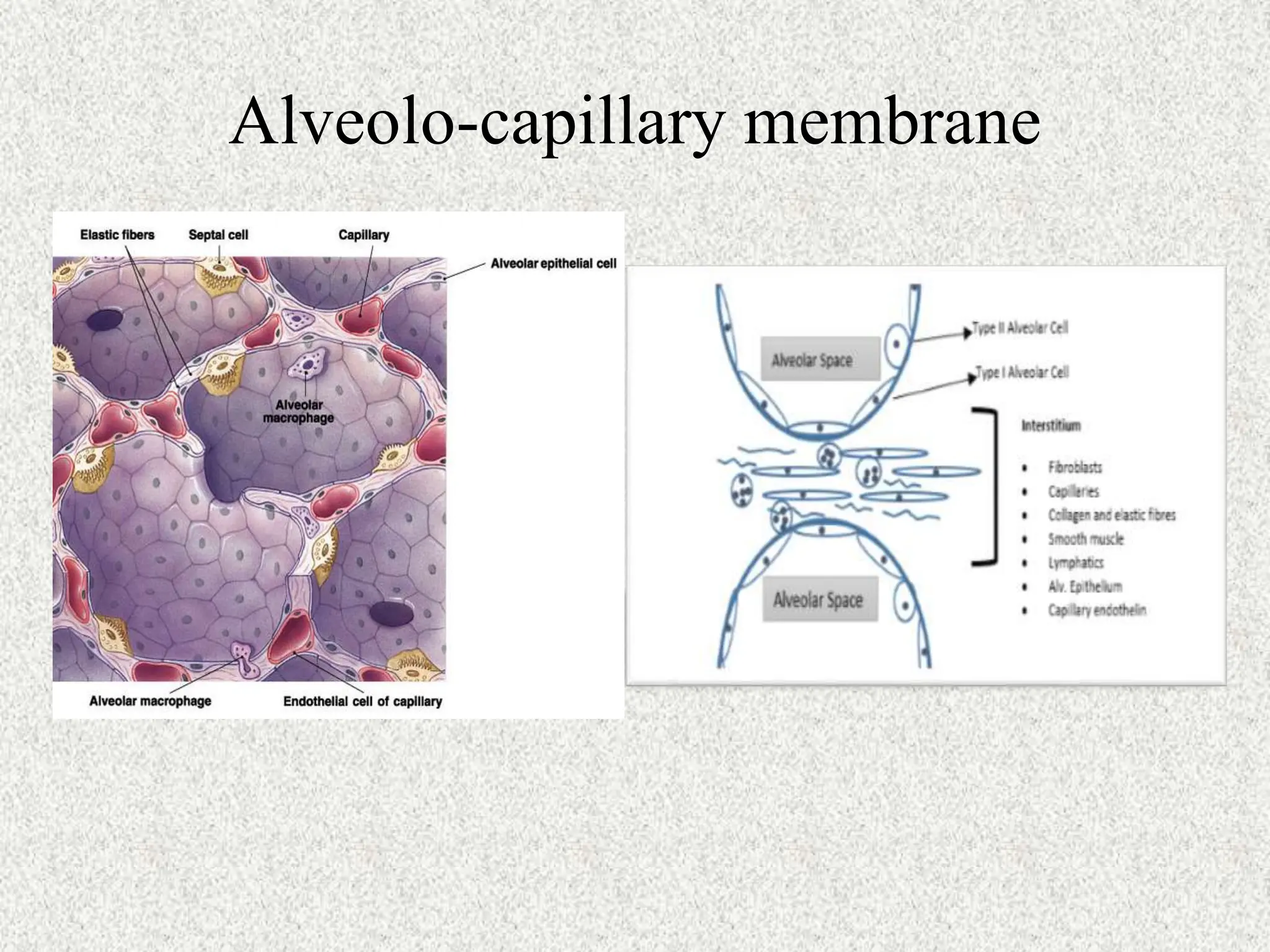
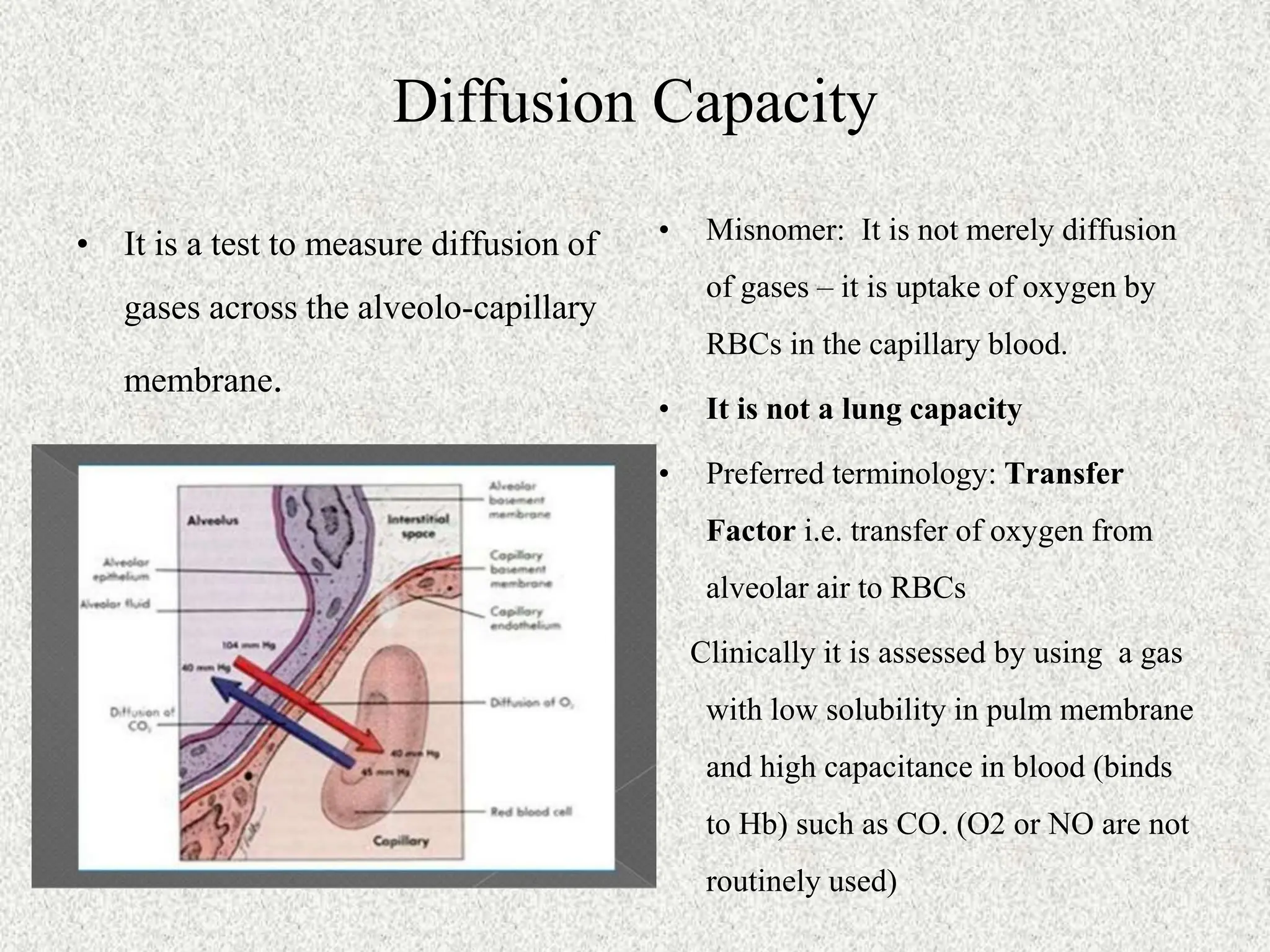
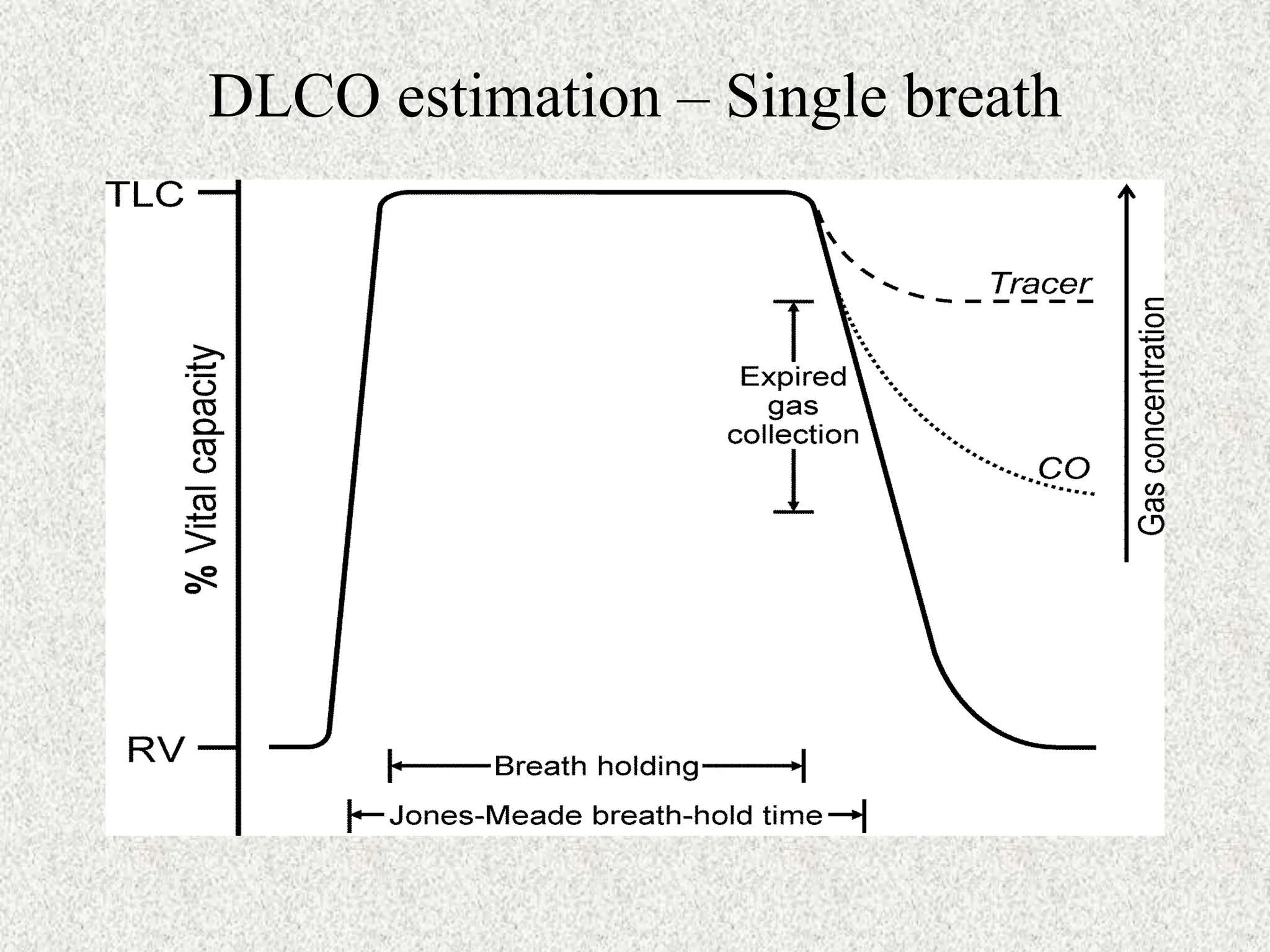
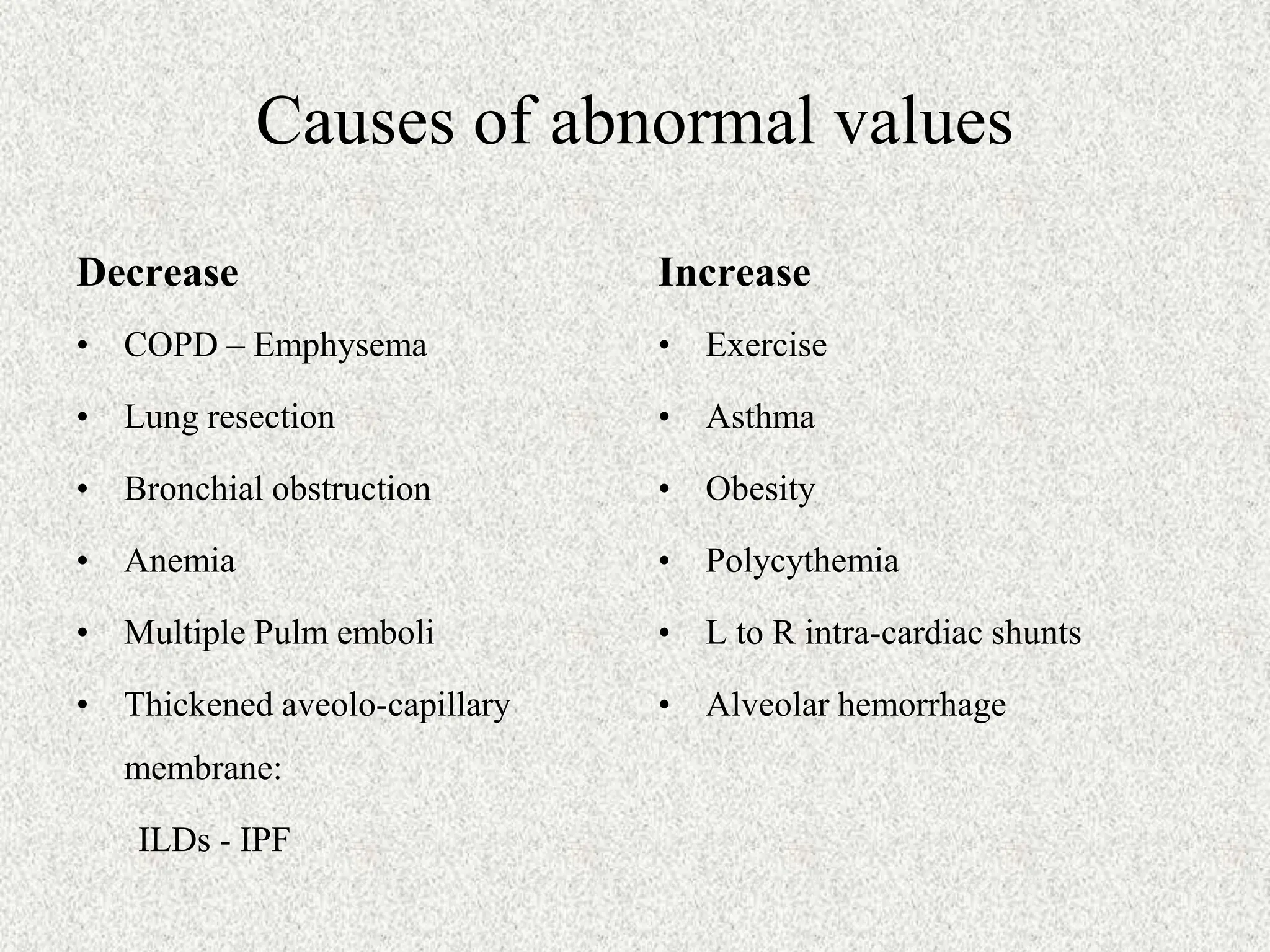
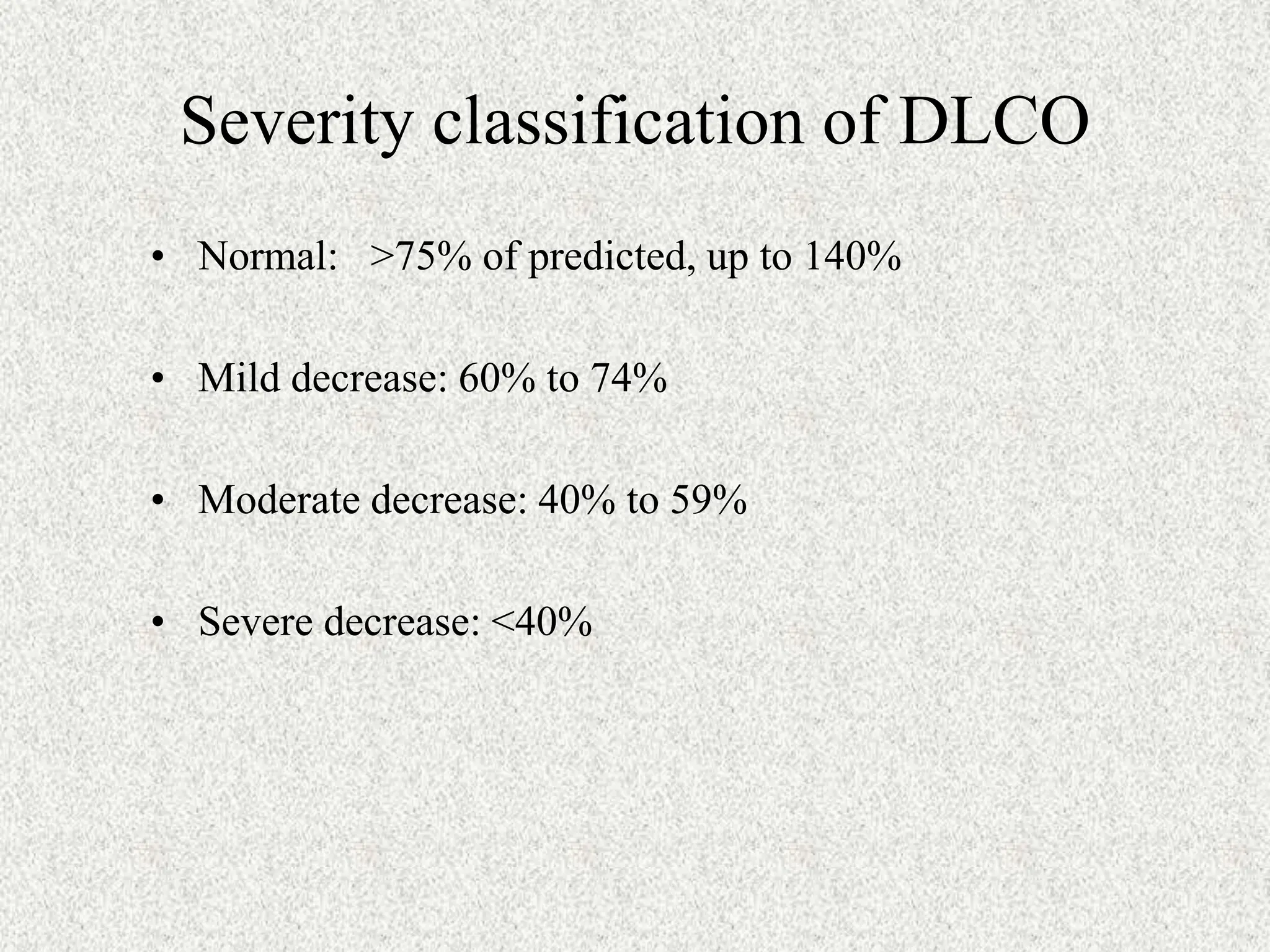
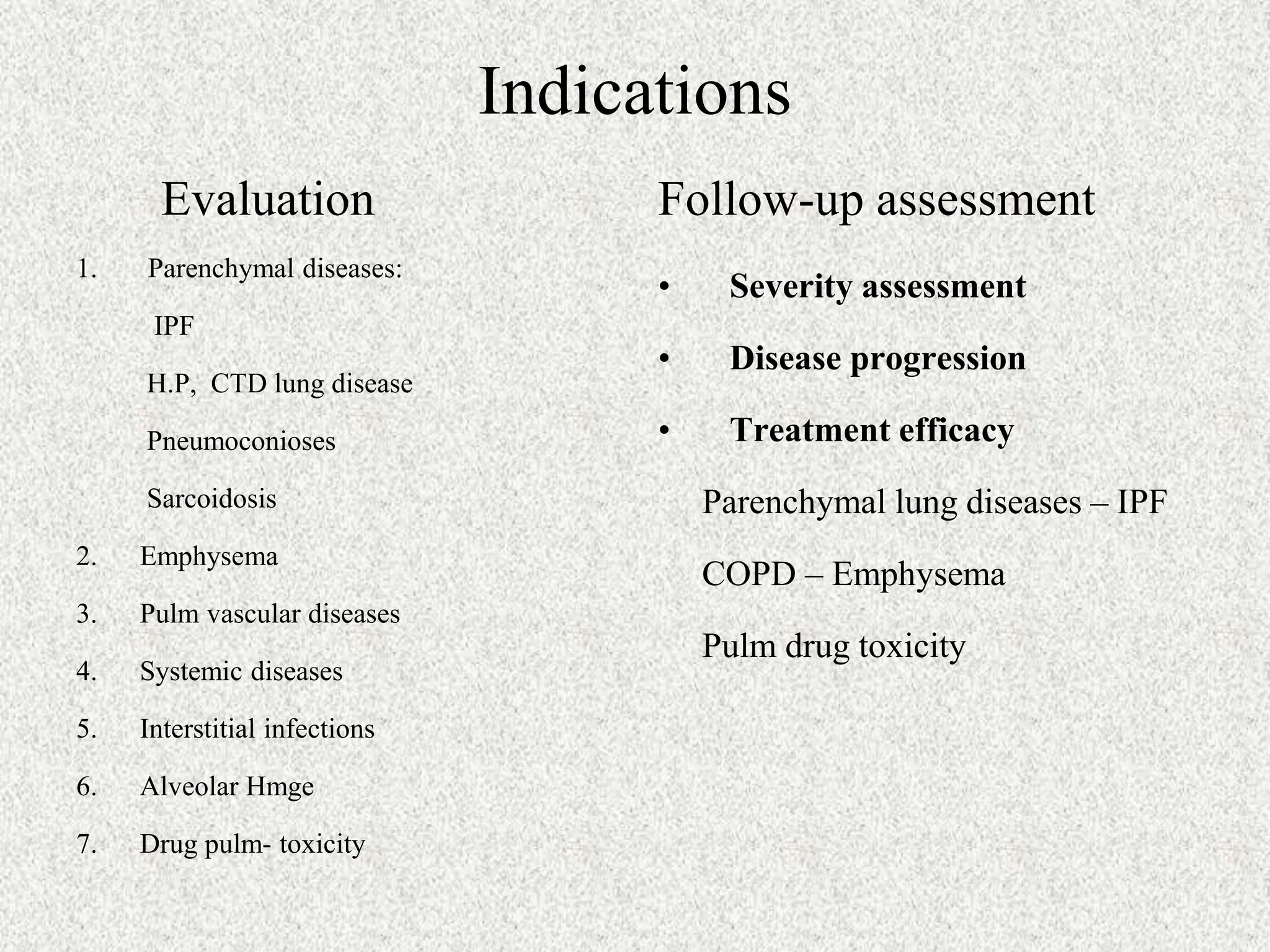
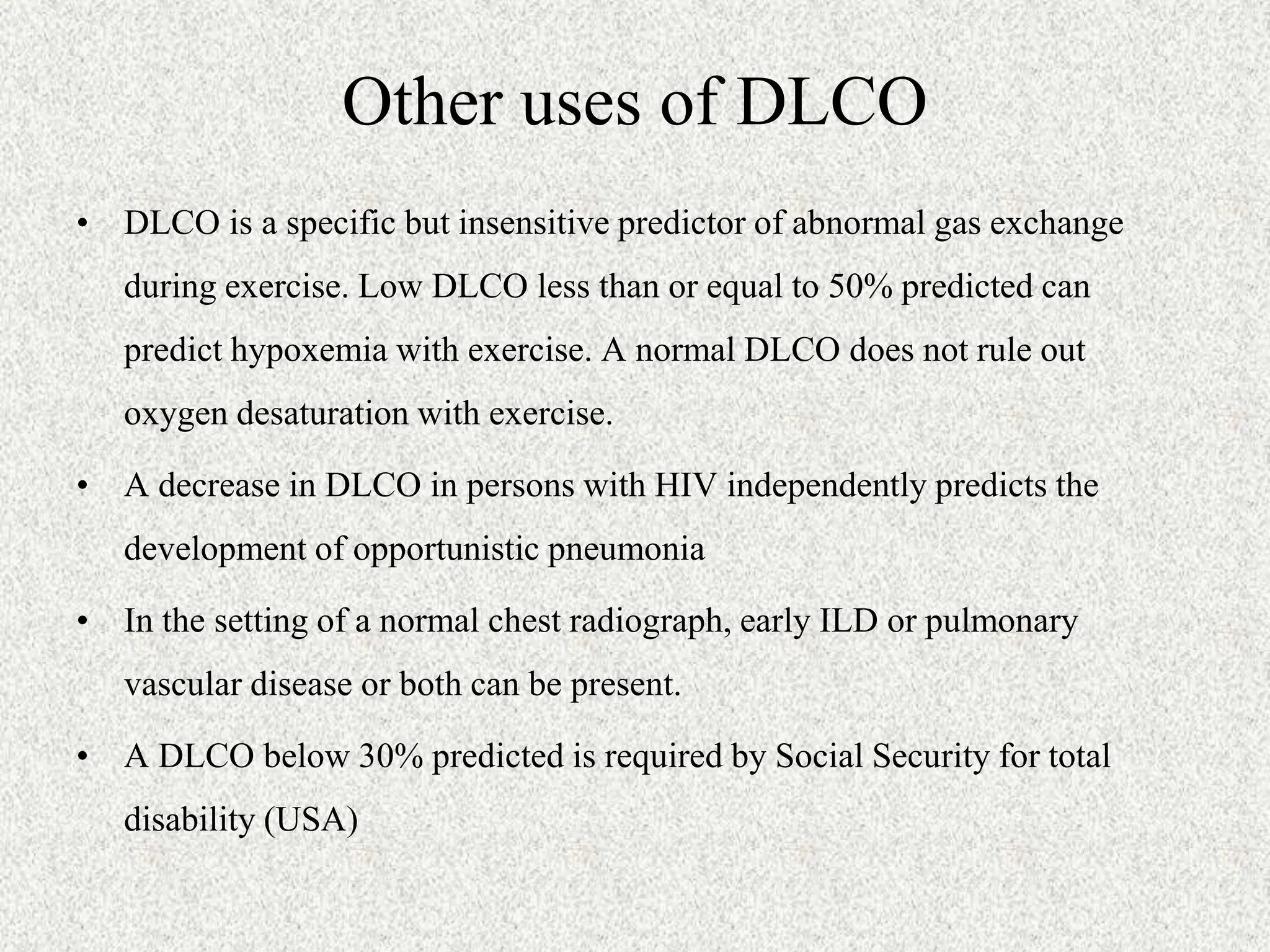
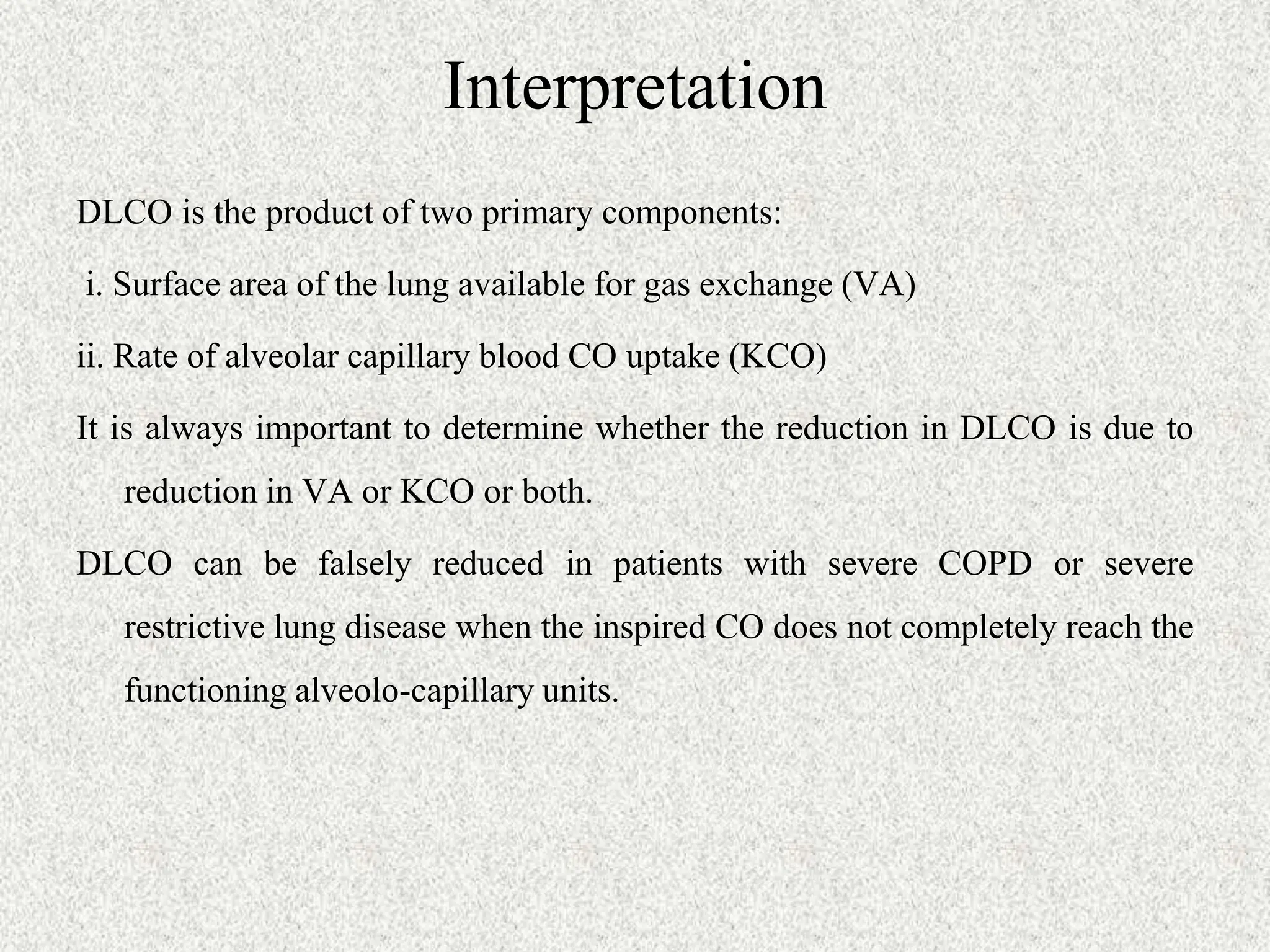
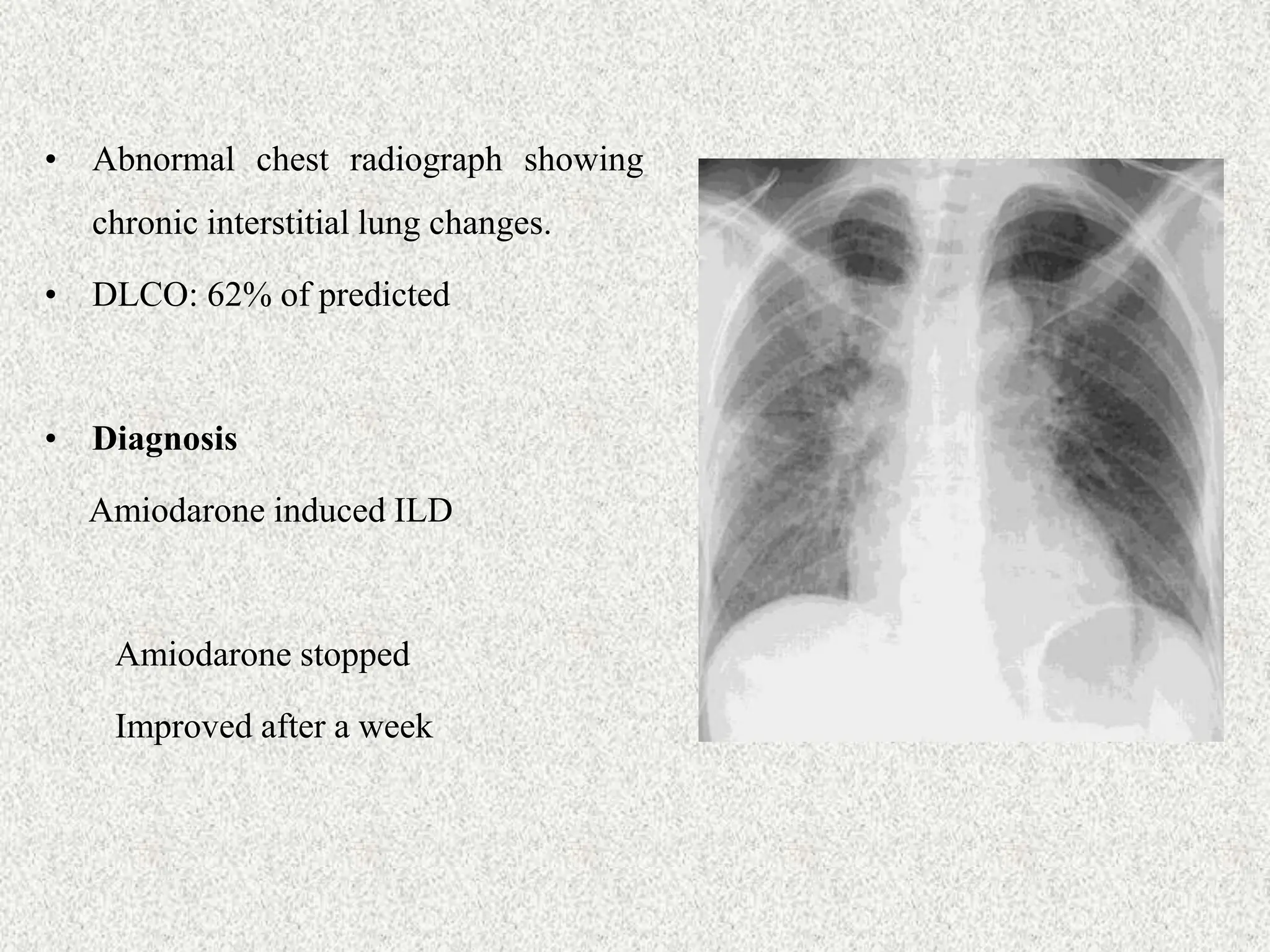
The document discusses the diffusion capacity (DLCO) test, which measures gas diffusion across the alveolo-capillary membrane, particularly the uptake of oxygen by red blood cells. It outlines determinants of normal and abnormal DLCO values, indications for evaluation, and interpretation of results, emphasizing its relevance in diagnosing parenchymal lung diseases and monitoring treatment efficacy. Additionally, it highlights potential pitfalls in DLCO testing and interpretation, stressing the importance of clinical context.