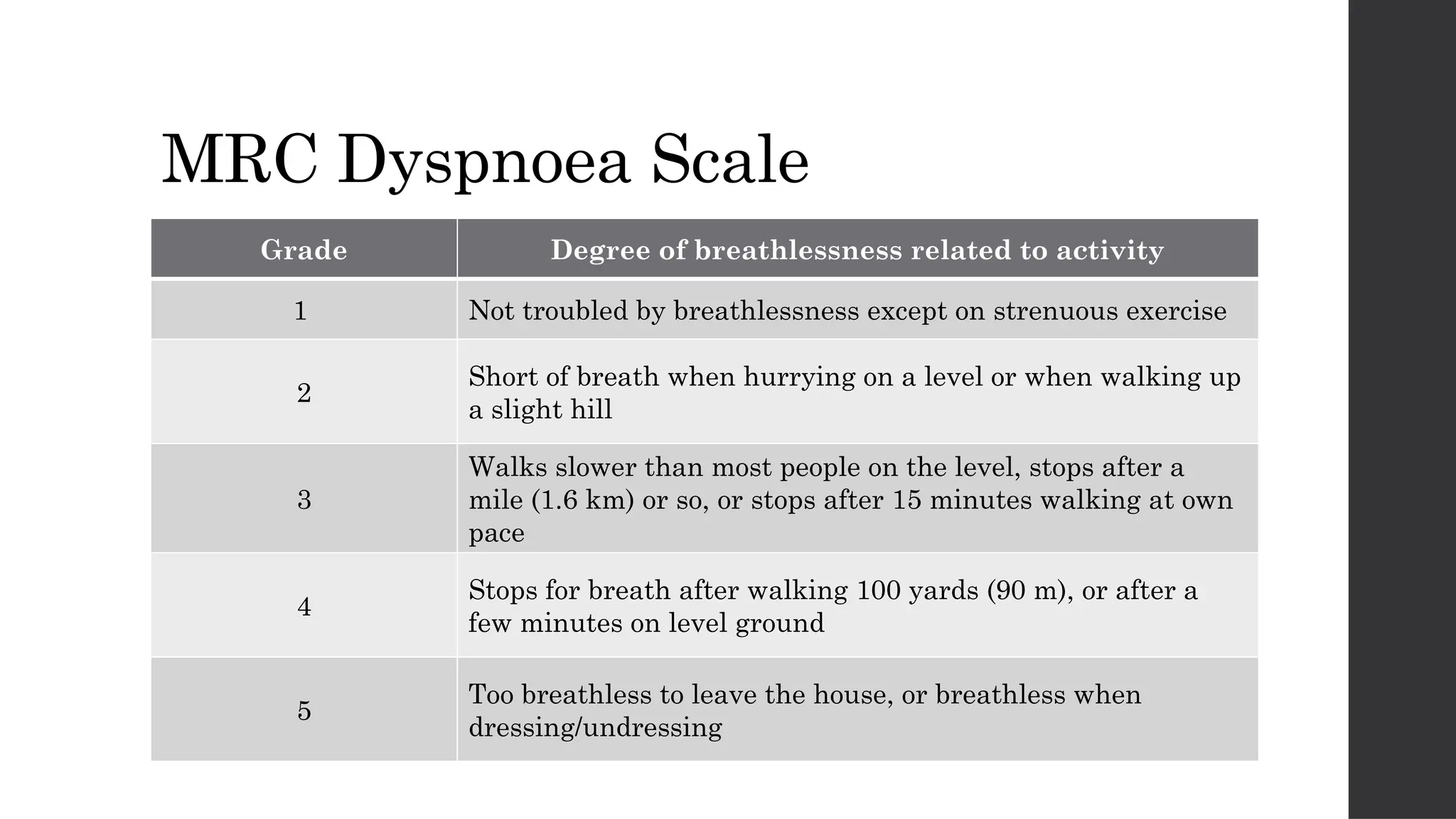
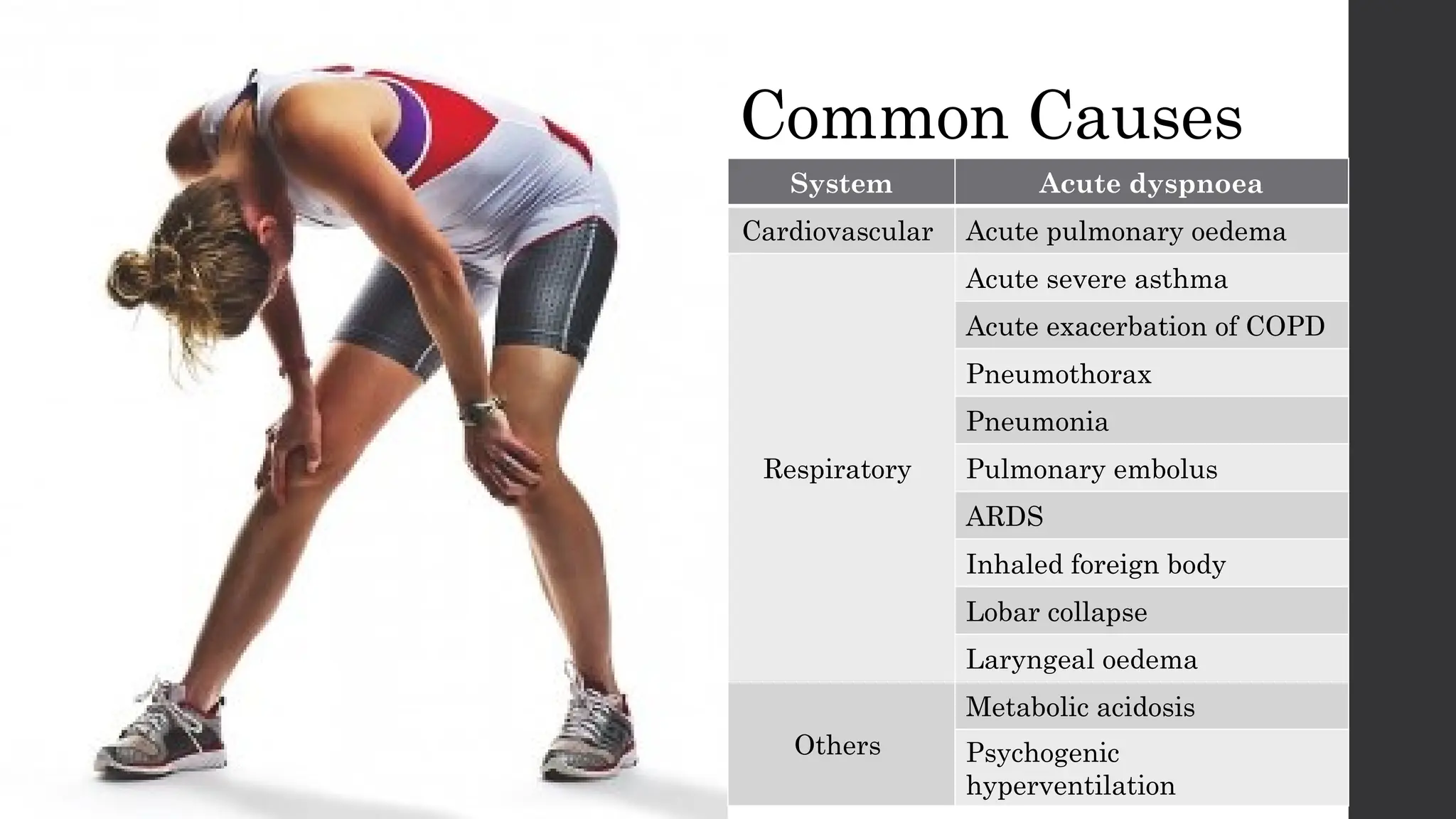
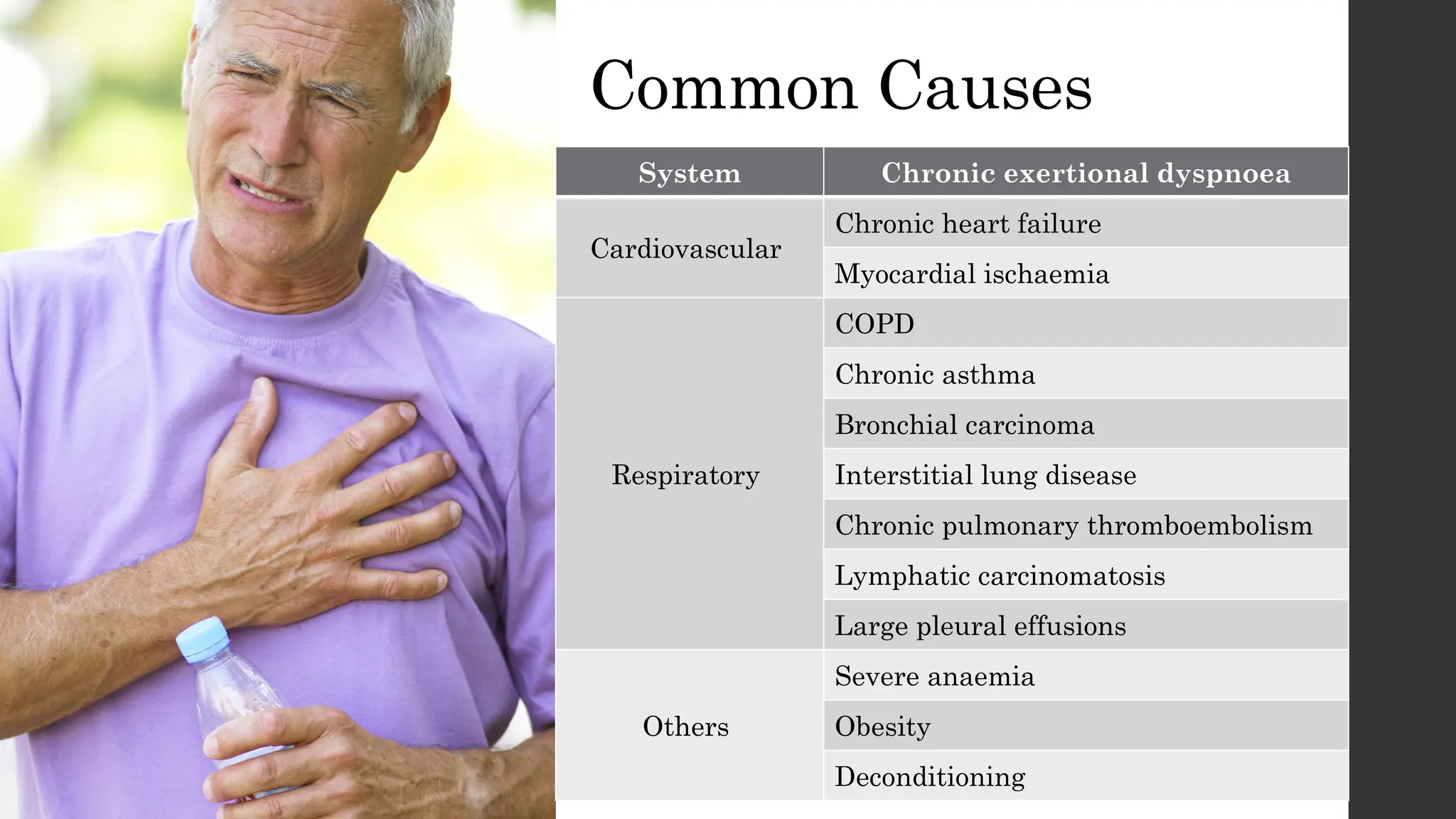
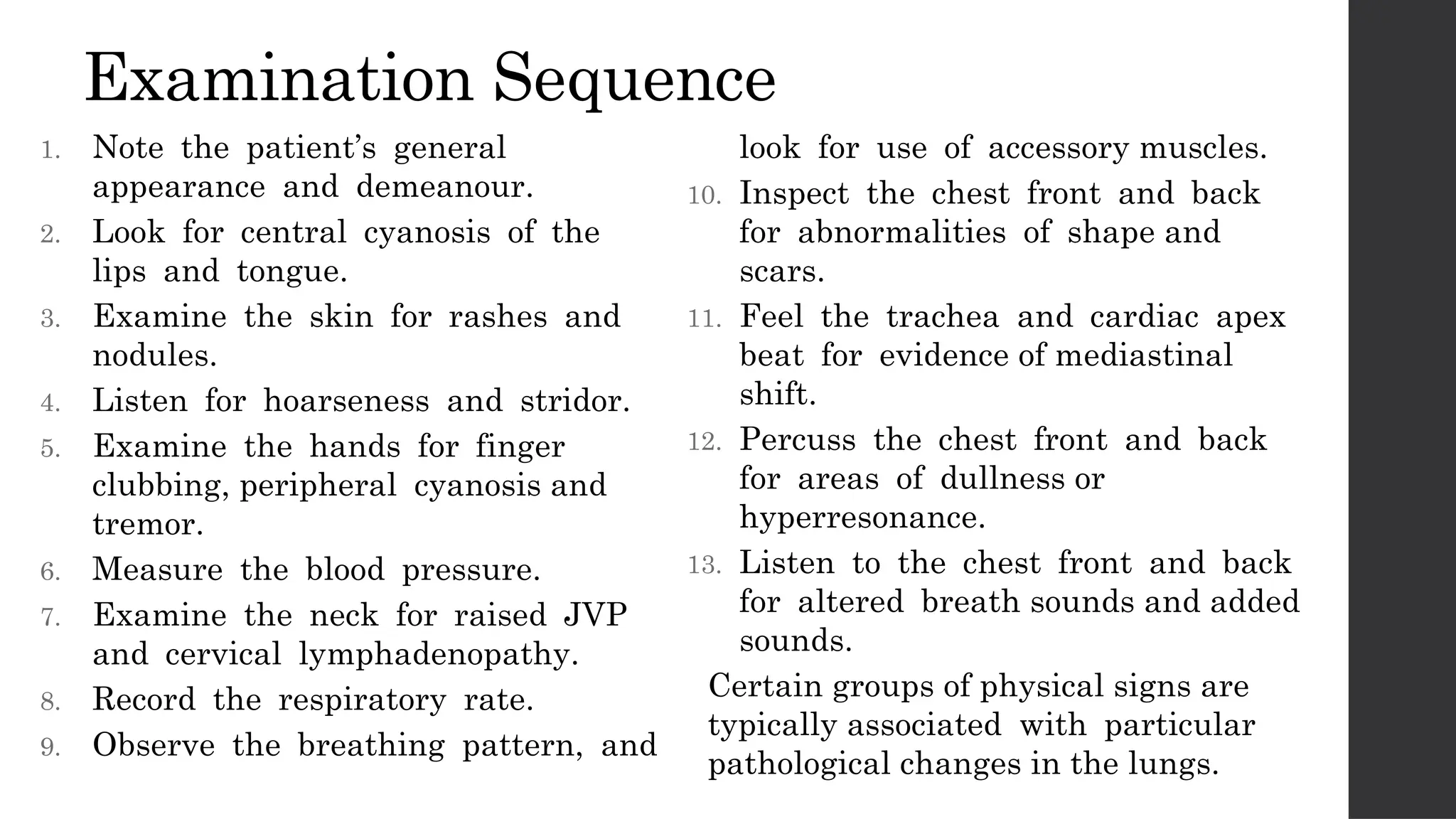
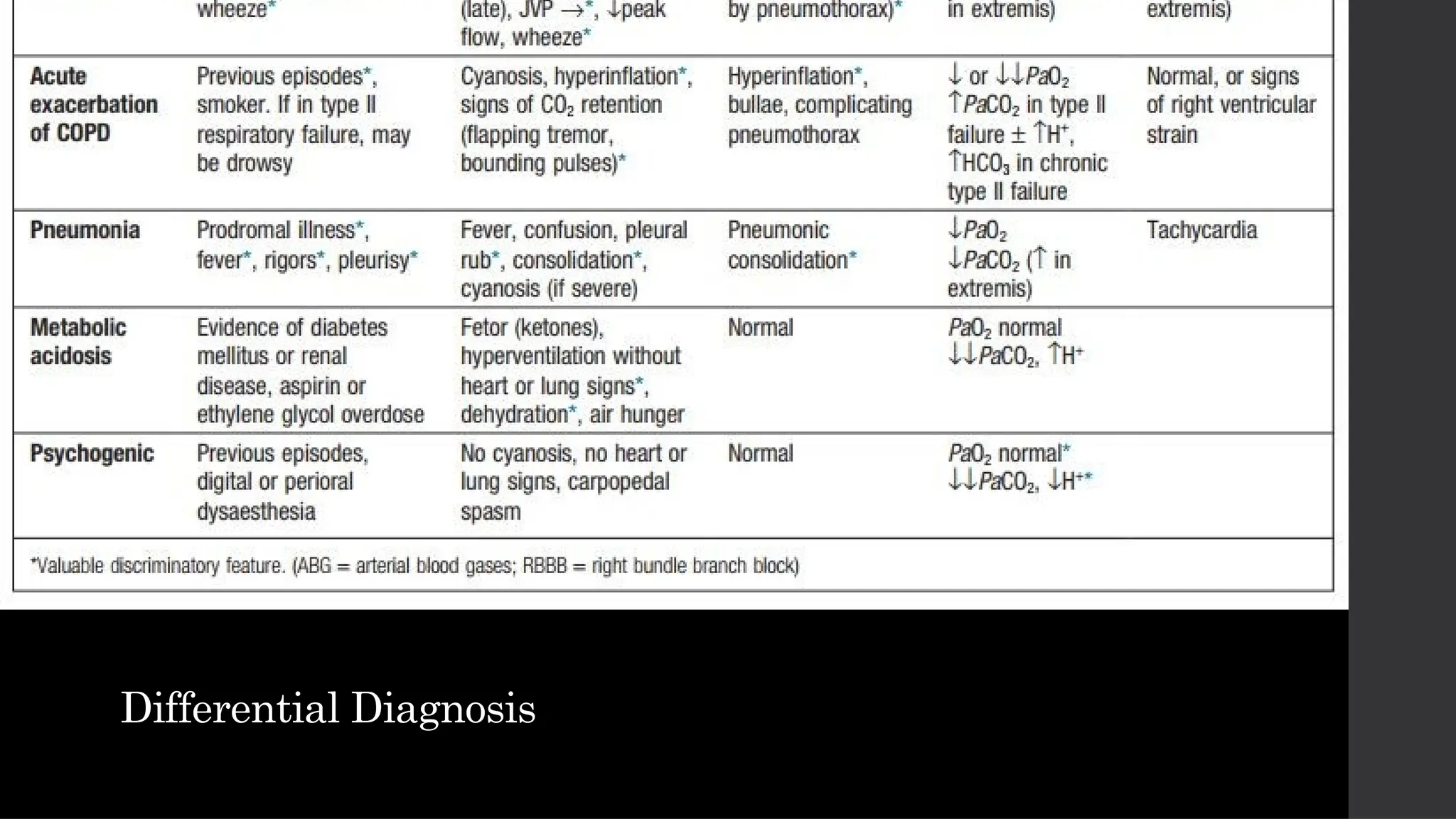
The document provides a comprehensive overview of shortness of breath, defining it as an uncomfortable need to breathe and detailing its various grades and common causes. It outlines essential historical and physical examination components for diagnosing dyspnea, along with initial investigations and management strategies. It emphasizes the importance of differential diagnosis, related investigations, and treatment options addressing both pharmacological and non-pharmacological approaches.