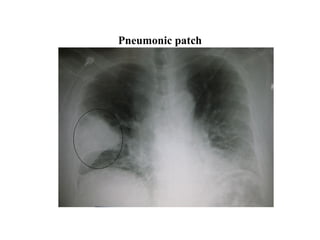
This document discusses various lung conditions including bronchiolitis obliterans, organizing pneumonia, and interstitial lung disease. It defines key terms and describes the symptoms, causes, diagnosis, and treatment of these conditions. Bronchiolitis obliterans involves scarring and obstruction of the bronchioles. Organizing pneumonia refers to unresolved pneumonia where exudates persist and cause fibrosis. Interstitial lung disease is a class of diffuse lung diseases involving inflammatory responses with varying degrees of pulmonary fibrosis. Specific forms like BOOP, COP, and IPF are mentioned along with their clinical presentation and pathological features.