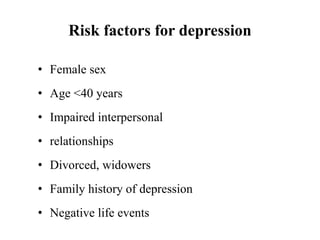
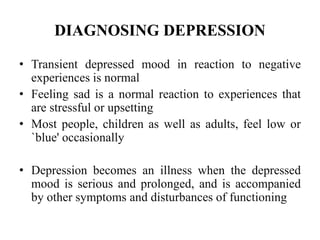
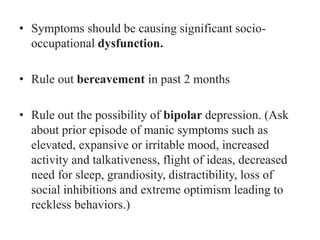
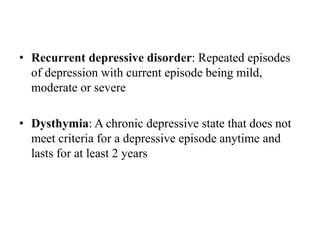
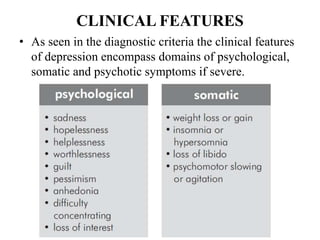
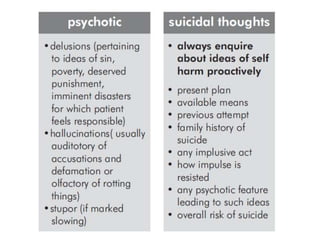
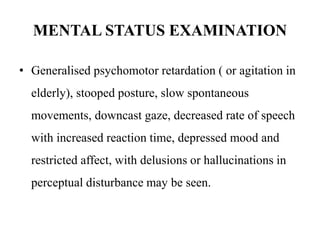
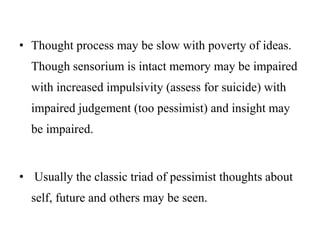
- Affective disorders include persistent mood disorders like depression that cause socio-occupational dysfunction. Depression is the most common mental disorder.
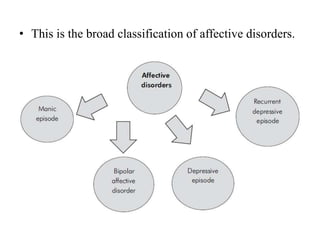
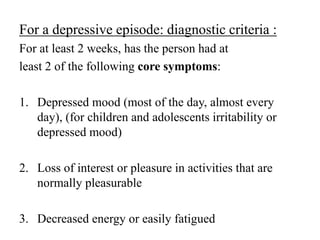
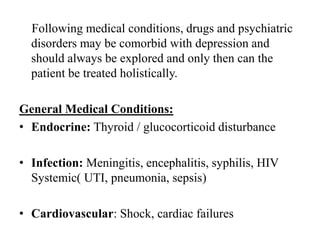
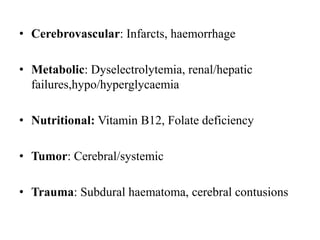
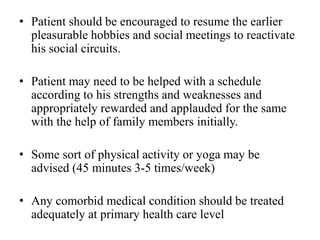
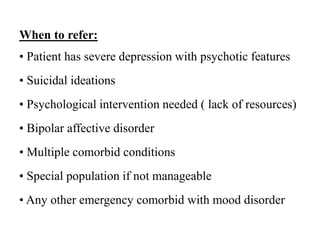
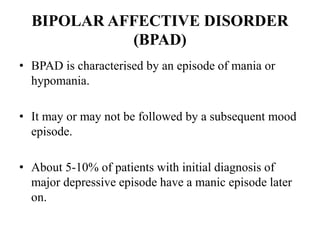
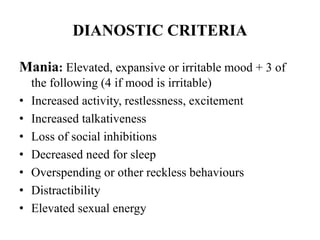
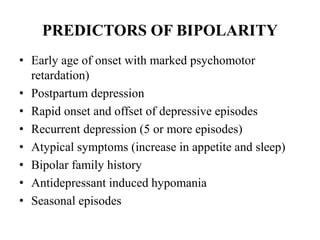
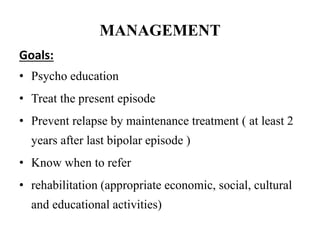
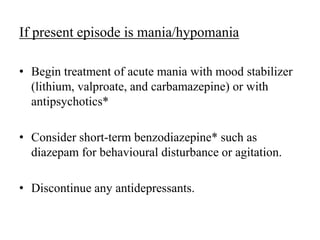
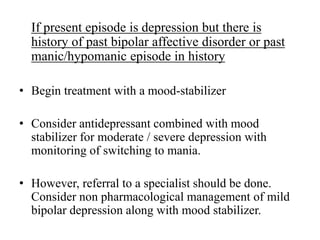
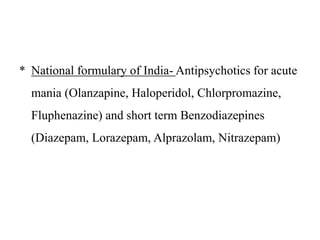
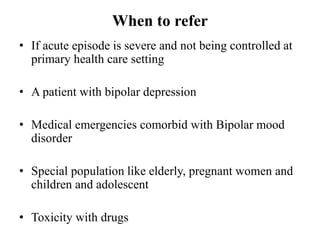
- The document outlines depression and bipolar affective disorder, their diagnostic criteria, clinical features, management, and when to refer patients. Depression is a leading cause of disability and its early identification and treatment improves outcomes. Bipolar disorder involves episodes of mania or hypomania with or without depression.