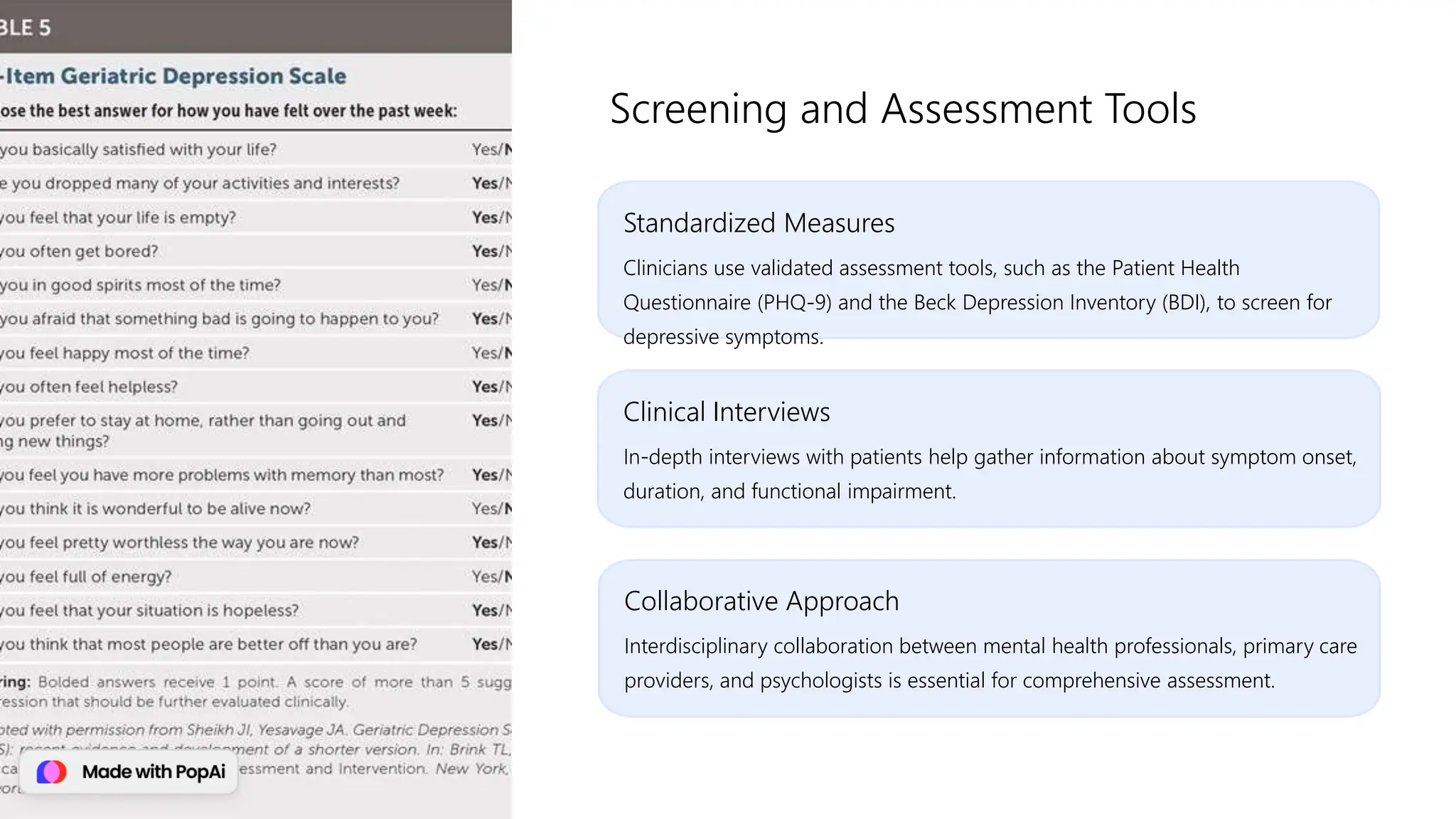
This document provides a comprehensive overview of depressive disorders, including definitions, prevalence, symptoms, risk factors, and types such as major depressive disorder and persistent depressive disorder. It discusses diagnosis criteria, assessment approaches, common comorbidities, and treatment options like medication and psychotherapy. Additionally, it emphasizes the importance of individualized care, lifestyle modifications, and integrated support models for effective management of depressive disorders.